Management of Specialty Work in COVID-19 - Do you have a solution?

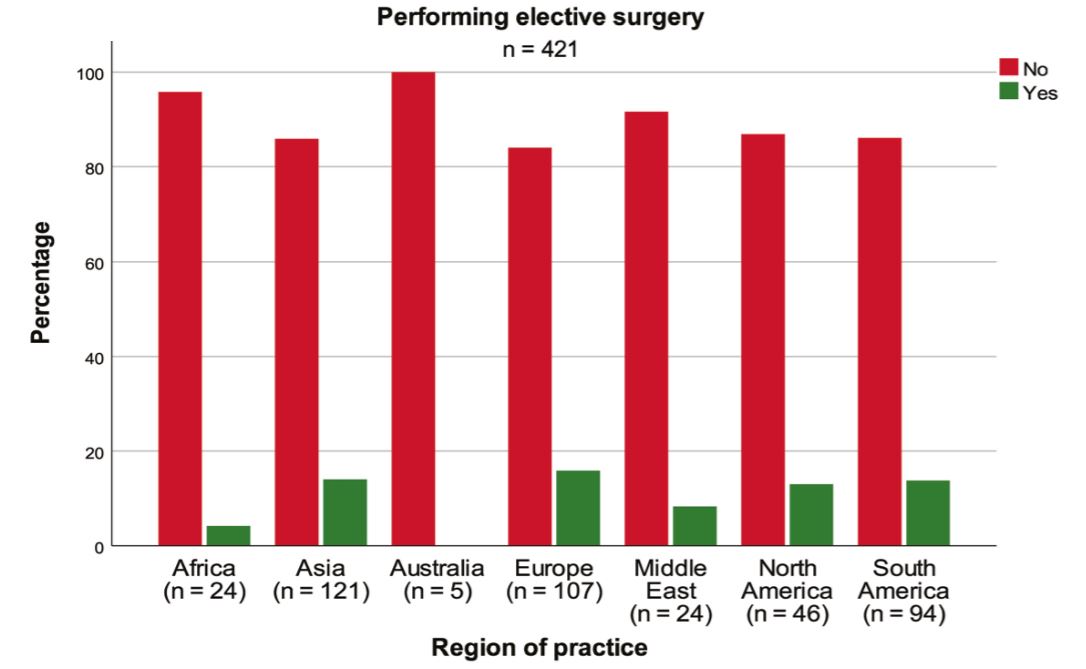
COVID-19 has changed the way many specialty services work internationally, however in low-and middle income countries, specialist care may not be readily available and healthcare professionals have to manage conditions across multiple specialties and disciplines to meet the need of the population. In addition, many countries have cancelled elective surgery to minimise risk during this pandemic.
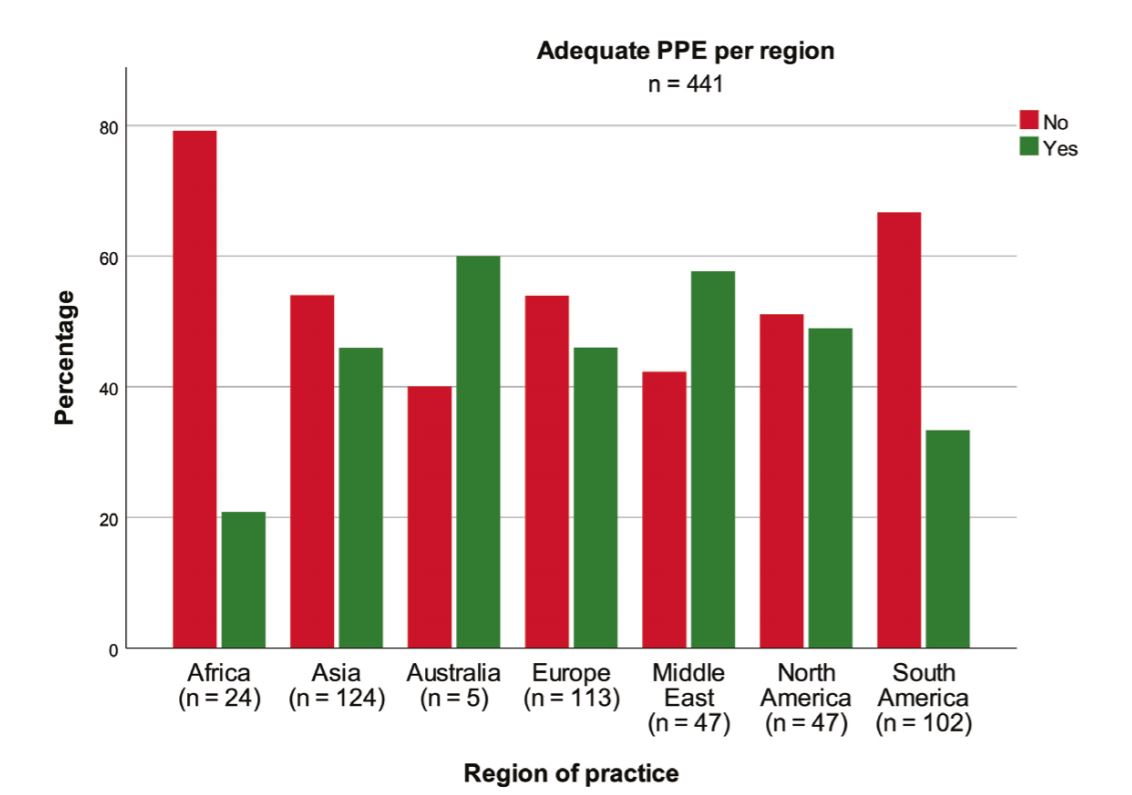
With many countries still dealing with new diagnoses of COVID-19, will PPE supplies be sufficient to restart elective and routine services?
Are healthcare professionals more at risk of getting COVID-19 due to the longer hours of exposure and need to care for COVID-19 patients? Research is still ongoing as to whether certain ethnic groups are at higher risk of COVID, confounding factors such as viral-load and variations in demographic representation in healthcare workers need to be taken into account when interpreting emerging data.
For further updates based on the recent analysis of UK Healthcare professional deaths see this article from the Health Service Journal.
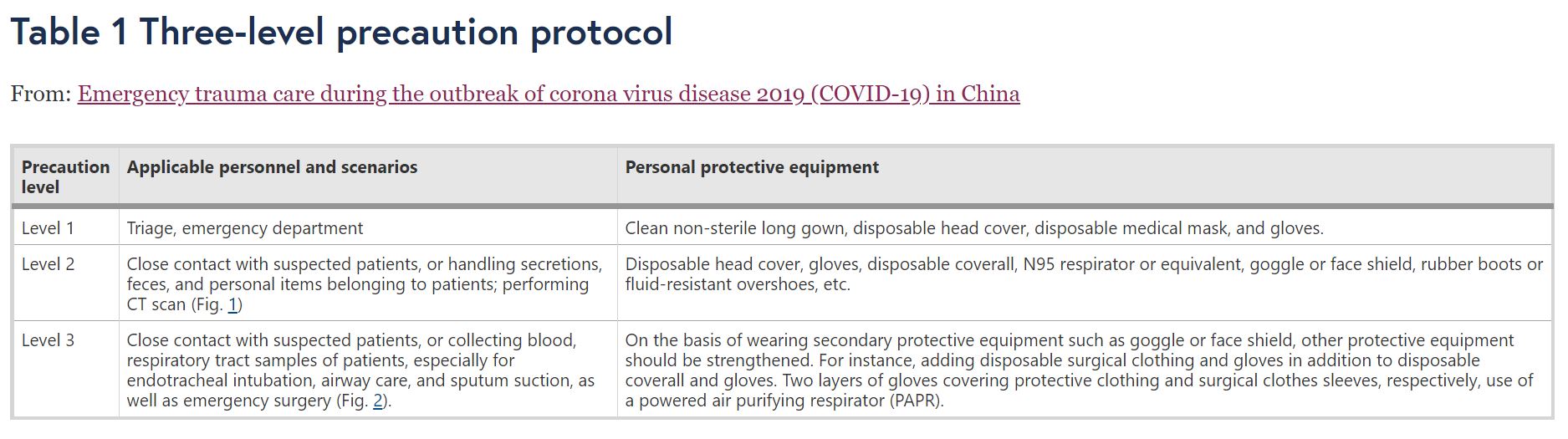
Triage systems have been put in place for emergency surgery, in order to manage PPE requirements and ensure the safety of healthcare staff.
Example: Recommendations from Li et al. (2020) : Emergency trauma care during the outbreak of corona virus disease 2019 (COVID-19) in China.
Special requirements for the hospitals receiving trauma patients during the outbreak
To control the spread of COVID-19, basic principles for treating infectious diseases should be followed, and necessary measures should be taken before receiving trauma patients.
Emergency department: Set up a triage area for assessment of all patients at admission, allowing early recognition of possible SARS-CoV-2 infection and immediate isolation of patients with suspected SARS-CoV-2 infection in an area separate from other patients.
Radiology department: A dedicated CT room should be kept on standby for the examination of infected patients.
Operating room (OR): A relatively isolated negative-pressure OR is preferable; if there is no permanent negative-pressure OR, a temporarily modified negative-pressure OR the main operating suite of the hospital can be converted.
Intensive care unit (ICU): An isolated area should be prepared in the ICU, and suspected patients should be treated in a single space.
Intrahospital transport: Although an ideal trauma center with a door-to-door CT room and negative-pressure OR are preferable in this situation, most regions in China do not operate such facilities. Therefore, a predetermined transport route should be used to minimize exposure, and any intrahospital transport should utilize dedicated carts demarcated by a warning logo equipped with protective supplies and hand disinfectants. The patient should wear a medical mask, and the walls and the floor of the passageways and the elevator should be covered with a plastic lining.
How specialty and elective services will restart and resume will be different across countries. However it is clear that this is not only a challenge for low and middle income countries, but a worldwide concern.
Read more on how LMIC could plan emergency and essential surgical services:
Emergency and essential surgical healthcare services during COVID-19 in low- and middle-income countries: A perspective
Share your experiences and comments
Don't forget to join MedShr's COVID-19 Africa or Middle East group today!
Loading Author...
Sign in or Register to comment