COVID-19 in Pregnancy

What do we know about COVID-19 in Pregnancy?
There is currently no evidence that pregnant women are at higher risk of contracting COVID-19 than the general population. However, physiological and immunological changes in pregnancy may mean that pregnant women may be adversely affected by respiratory infections [1].
In the UK, pregnant women with existing co-morbidities have been included in the “shielded group”, where they are advised to self-isolate even without COVID-19 symptoms [2].
In low and middle income countries (LMIC), many women may attend their local delivery units or health posts which may not have facilities such as C-section and specialist medical support [3]. In such regions, where maternal and perinatal mortality rates are still a concern, what do we know about COVID-19 that can help us support women in pregnancy and perinatal care in a COVID-19 pandemic?
Key points from Literature:
• In a review of current literature by Mullins et al. (2020),29 women with COVID-19 delivered 30 infants (one twin pregnancy), majority by C-section and two by vaginal delivery[3]
• From small case series on COVID-19 in pregnancy, maternal, fetal, and neonatal outcomes were good in those with mild infections [5]
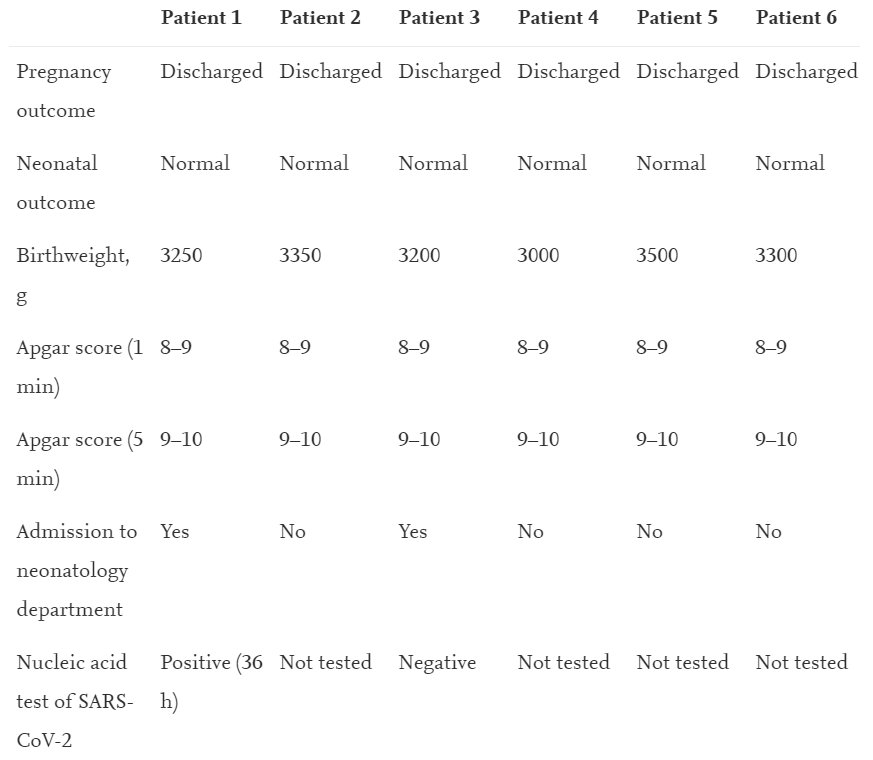
• Yu et al. (2020) reported their series of 7 patients from Wuhan, who were diagnosed with COVID-19 during pregnancy. Their average gestation was 39 weeks plus 1 day (range 37 weeks to 41 weeks plus 2 days) at admission, and all patients had mild symptoms with no ICU admissions [5]
• Juusela et al. (2020) reported 2 cases of cardiomyopathy in COVID-19 pregnant patients, viral myocarditis and cardiomyopathy have been reported in non-pregnant COVID-19 patients, not enough is know whether there is an increased risk of cardiomyopathy in pregnancy [6]
• Breslin et al (2020) reported 2 pregnant patients with COVID-19, though asymptomatic at presentation, ultimately required unplanned ICU admission for COVID-19 respiratory complications [7]
• Characteristics of COVID-19 presented in the same way in pregnancy as in non-pregnant patients, including no symptoms in early stages [5, 7]
• However there is still no reliable evidence recommending any specific COVID-19 treatment for pregnant women [5]
• WHO guidance does not recommend the use of corticosteroids for COVID-19 [8,9]
• There is little evidence on prone positioning in pregnant women with ARDS but this could be considered in early pregnancy, instead in the third trimester, they may benefit from being in the lateral decubitus position [10]
Maternal presenting symptoms of COVID-19: Average incubation time = 5 days (range 2–9 days)
1) Fever (86%)
2) Cough (14%)
3) Shortness of breath/ breathing difficulty (14%)
4) Gastrointestinal symptoms (14%)
Example of discharge criteria for postpartum patients (From Yu et al. (2020) [5]):
Normal body temperature >3 days
Improved respiratory symptoms
Chest imaging showing significant improvement in acute exudative lesions
Negative nucleic acid test of respiratory specimens such (sputum and nasopharyngeal swabs) twice in a role when sampled >24h apart
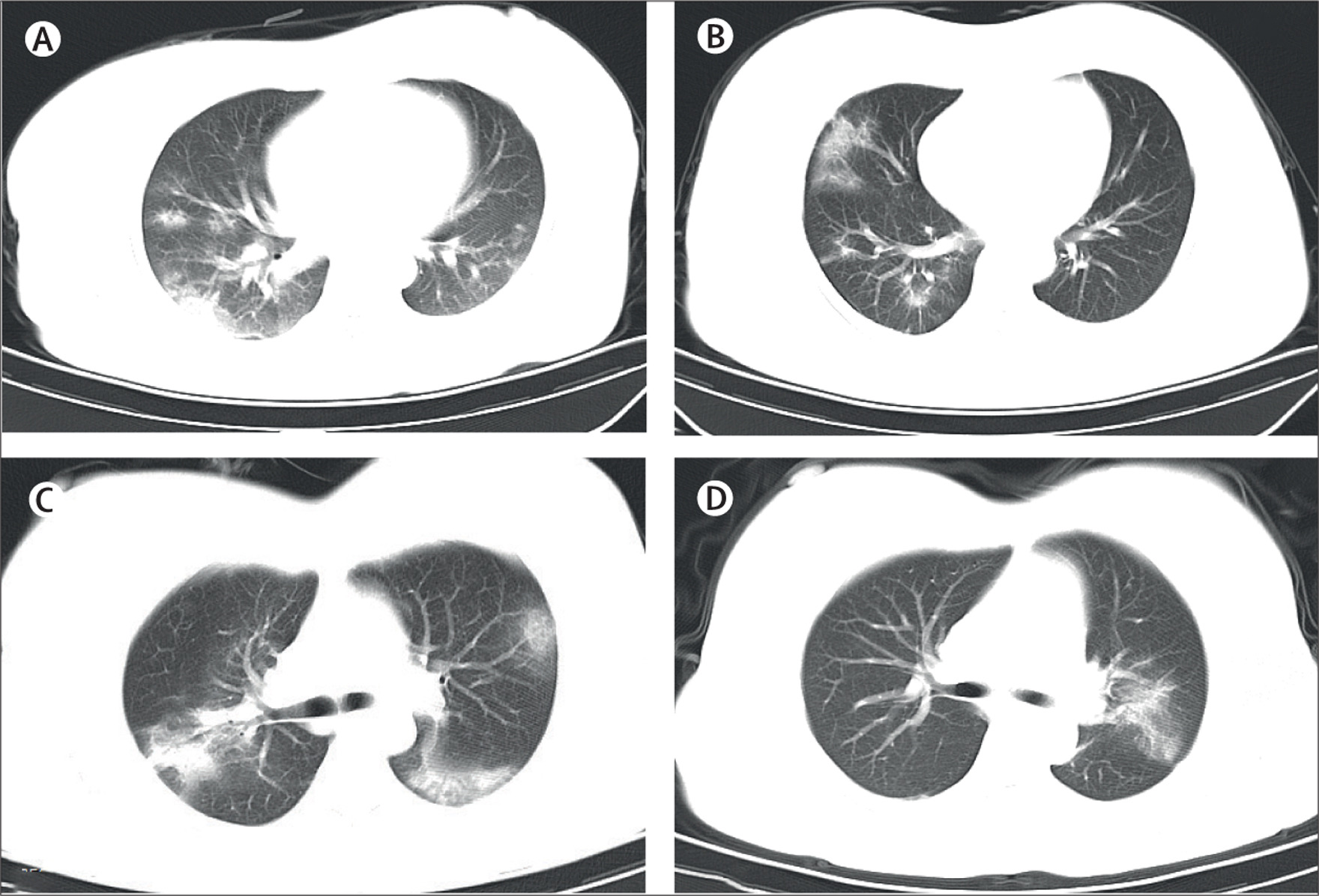
Image Source: Yu et. al. (2020)
Chest CT of 4 pregnant patients admitted with COVID-19, showing bilateral large areas of multiple ground-glass opacities or patchy shadow with an uneven density
For more information on COVID-19 in pregnancy and breastfeeding view the WHO Q&A pages here: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub
First Published 8 April 2020
Last Updated: 10 June 2020
References:
1. WHO, 2020, Q&As on COVID-19 and related health topics (Website), URL: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub (accessed 10/6/2020)
2. NHS Digital, Last updated 21 May 2020, Coronavirus (COVID-19): Shielded patients list, Accessed 29/5/2020, URL: https://digital.nhs.uk/coronavirus/shielded-patient-list
3. Cavallaro FL, Benova L, Dioukhane EH, et al.,What the percentage of births in facilities does not measure: readiness for emergency obstetric care and referral in Senegal, BMJ Global Health 2020;5:e001915.
4. Mullins E, Evans D, Viner RM, O'Brien P, Morris E. Coronavirus in pregnancy and delivery: rapid review. Ultrasound Obstet Gynecol. 2020;55(5):586‐592. doi:10.1002/uog.22014
5. Nan Yu, Wei Li, Qingling Kang, Zhi Xiong, Shaoshuai Wang, Xingguang Lin, Yanyan Liu, Juan Xiao, Haiyi Liu, Dongrui Deng, Suhua Chen, Wanjiang Zeng, Ling Feng, Jianli Wu (2020), Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: a retrospective, single-centre, descriptive study, The Lancet Infectious Diseases, https://doi.org/10.1016/S1473-3099(20)30176-6
6. Juusela A, Nazir M, Gimovsky M, Two Cases of COVID-19 Related Cardiomyopathy in Pregnancy., American Journal of Obstetrics & Gynecology MFM (2020), doi: https:// doi.org/10.1016/j.ajogmf.2020.100113
7. Breslin N, Baptiste C, Miller R, Fuchs K, Goffman D, Gyamfi-Bannerman C, D’Alton M, COVID-19 in pregnancy: early lessons, American Journal of Obstetrics & Gynecology MFM (2020), doi: https://doi.org/10.1016/j.ajogmf.2020.100111
8. WHO (2020), Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected: interim guidance. URL: https://www.who.int/docs/default-source/coronaviruse/clinical-management-of-novel-cov.pdf (accessed 6/4/2020)
9. WHO (2020), Novel coronavirus—China. (Website) URL: http://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/ (accessed 6/4/2020)
10. WHO (2020), Clinical management of COVID-19: interim guidance, (Website) URL:https://www.who.int/publications/i/item/clinical-management-of-covid-19 (Accessed 10/6/2020)
Loading Author...
Thank you that was very useful and reassurring to me as a obstetrician