NICE COVID-19 RAPID Guideline - Critical Care
1. Admission to hospital
1.1On admission to hospital, assess all adults for frailty, irrespective of age and COVID‑19 status. Consider comorbidities and underlying health conditions.
Use the Clinical Frailty Scale (CFS) for frailty assessment, available from the NHS Specialised Clinical Frailty Network.
Record the frailty assessment in the patient's medical record.
1.2When patients with possible COVID‑19 have been identified, follow appropriate UK government guidance on infection prevention and control measures. This includes recommendations on:
patient transfers and transport
segregation and cohorting
personal protective equipment
aerosol-generating procedures.
1.3If COVID‑19 is diagnosed in someone not isolated from admission or presentation, follow UK government guidance on actions required when a case was not diagnosed on admission.
2. Admission to critical care
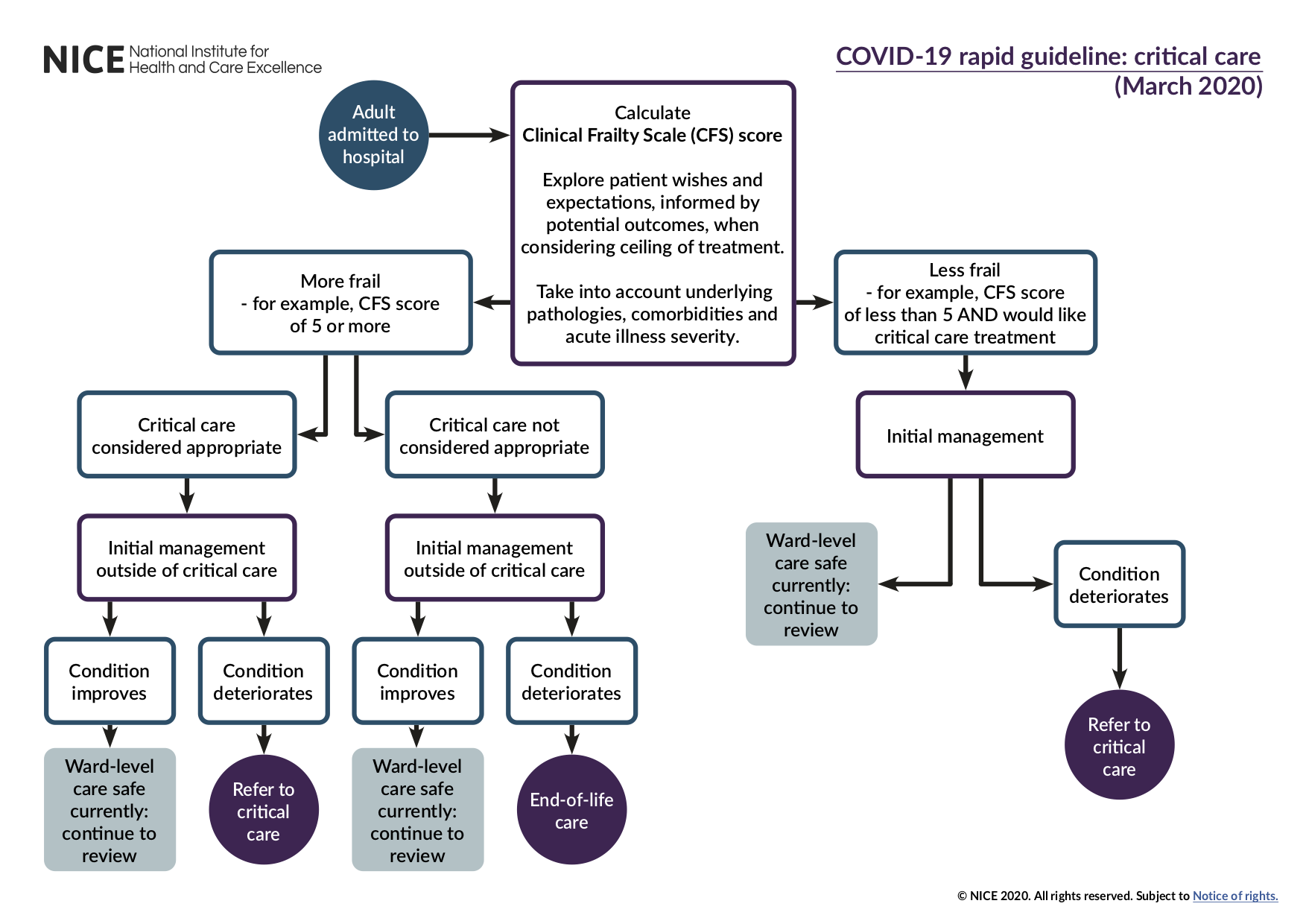
See the critical care admission algorithm.
2.1Discuss the risks, benefits and possible likely outcomes of the different treatment options with patients, families and carers using decision support tools (where available) so that they can make informed decisions about their treatment wherever possible. See information to support decision making.
2.2Involve critical care teams in discussions about admission to critical care for a patient where:
the CFS score suggests the person is less frail (for example the score is less than 5), they are likely to benefit from critical care organ support and they want critical care treatment or
the CFS score suggests the person is more frail (for example the score is 5 or more), there is uncertainty regarding the likely benefit of critical care organ support, and critical care advice is needed to help the decision about treatment.
Take into account the impact of underlying pathologies, comorbidities and severity of acute illness on the likelihood of critical care treatment achieving the desired outcome.
2.3Support non-critical care healthcare professionals to discuss treatment plans with patients who would not benefit from critical care treatment or who do not wish to be admitted to critical care.
2.4Sensitively discuss a possible 'do not attempt cardiopulmonary resuscitation' decision with all adults with capacity and a CFS score suggestive of increased frailty (for example of 5 or more). Include in the discussion:
the possible benefits of any critical care treatment options
the possible risks of critical care treatment options
the possible likely outcomes.
Involve a member of the critical care team if the patient or team needs advice about critical care to make decisions about treatment.
2.5Ensure healthcare professionals have access to resources to support discussions about treatment plans (see for example decision-making for escalation of treatment and referring for critical care support, and an example decision support form).
2.6Ensure that when treatment outside critical care is the agreed course of action, patients receive optimal care within the ward.
3. Starting, reviewing and stopping critical care treatment
3.1Start critical care treatment with a clear plan of how the treatment will address the diagnosis and lead to agreed treatment goals (outcomes).
3.2Review critical care treatment regularly and when the patient's clinical condition changes. Include in the review an assessment of whether the goals of treatment are clinically realistic.
3.3Stop critical care treatment when it is no longer considered able to achieve the desired overall goals (outcomes). Record the decision and the discussion with family and carers, the patient (if possible) or an independent mental capacity advocate (if appropriate).
4. Clinical decision-making
4.1Be aware that guidance on treating COVID‑19 may change with emerging scientific data and knowledge and that this may require modifications to treatment.
4.2Base decisions on admission of individual adults to critical care on the likelihood of their recovery, taking into account the likelihood that a person will recover from their critical care admission to an outcome that is acceptable to them.
4.3Support all healthcare professionals to use their existing knowledge and experience when making clinical decisions.
4.4Critical care staff should support healthcare professionals who do not routinely work in critical care but need to do so (see guidance from the Faculty of Intensive Care Medicine).
4.5Decisions about the use of critical care resources should only be made by, or with the support of, healthcare professionals with expert knowledge and skills in critical care.
4.6Use objective data from recognised national sources, for example, the Intensive Care National Audit Research Centre, to support consistency in decision-making.
4.7Use a recognised tool to record the decision-making process (see an example decision support form).
5 Service organisation
Providing telephone advice
5.1Trusts should review their 'management of the deteriorating patient' strategy and use of the track and trigger system (NEWS2 has been endorsed by NHS England/Improvement) to allow for telephone advice rather than face-to-face review from critical care when clinically appropriate. See the NICE guideline on acutely ill adults in hospital for recommendations on identifying patients whose clinical condition is deteriorating or is at risk of deterioration.
5.2Document referral to and advice from critical care services in a standard format. Where telephone advice from critical care is appropriate this should still be documented in a standard format (see an example of a tool for documentation).
Coordinating best use of critical care resources
5.3Hospitals should discuss the sharing of resources and the transfer of patients between units, including units in other hospitals, to ensure the best use of critical care within the NHS.
5.4Data on the availability of critical care beds should be made available to the critical care decision makers and operational management team to facilitate sharing of resources (see table 1 for information on maximising critical care bed usage).
Table 1 Maximising critical care bed usage
Within critical care
Have all patients in critical care been reviewed with clear management plans established for the next 24 hours?
Can any level 2 or level 3 capacity be established in other areas of the hospital?
Can care suitable for particular patients be delivered in any other location - for example, can an enhanced care facility be created?
Are you aware of any capacity in neighbouring units within the network or out of the network?
Can any patients be transferred to other units to improve flow?
Outside critical care
Do you know what demand is occurring or is likely to occur in the rest of the hospital?
Do you know the number of patients for whom escalation to critical care is planned (if required)?
5.5Include Operational Delivery Networks and equivalent in discussions of mutual aid to ensure patients have access to all available, relevant critical care resource.
Extracorporeal membrane oxygenation
5.6Be aware that respiratory extracorporeal membrane oxygenation (ECMO) services can advise intensive care clinicians on managing severe acute respiratory failure.
5.7Be aware that respiratory ECMO services can accept referrals for critically ill patients where:
they have potentially reversible severe respiratory failure
optimal conventional intensive care management has failed
they meet the eligibility criteria for the respiratory ECMO service.
For more information see Management of surge and escalation in critical care services: standard operating procedure for adult respiratory extra corporeal membrane oxygenation.
Loading Author...
Sign in or Register to comment