Long-term Effects of COVID-19: Long COVID
Open article published on MedShr: 26th November 2020
Last updated: 26th November 2020
Every effort has been made to ensure that the information contained in this article is accurate and current at time of publication, but if you notice an error please contact covid@medshr.net and we will aim to address this. Please find MedShr’s full terms of service here.
Long COVID - Origins and Nomenclature
At time of publishing this article, it is reported that over 38.5 million patients have recovered from COVID-19 infection globally.[1] However, since early in the pandemic, there has been a growing awareness of the significant proportion of people affected by SARS-CoV-2 who have symptoms persisting well beyond the early (acute) phase of the infection.[2] Patients have played a central role in promoting an awareness of these symptoms.[3]
This pattern of symptoms has been termed ‘post-acute COVID-19’ (or similar) in scientific literature, but increasingly is recognised by the term Long COVID. The origin and evolution of the term Long COVID - which was created by patients experiencing persistent symptoms following an illness in with keeping COVID-19 infection - has been explored in this short communication, “How and Why Patients Made Long Covid”.[3]
The underlying aetiology(ies) and risk factors are not yet clearly understood, although comparisons have been drawn to sequelae in post-viral fatigue syndrome, myalgic encephalomyelitis (chronic fatigue syndrome), and patterns from other pandemics including SARS and MERS (see summary in Greenhalgh et al. 2020).[2, 4]
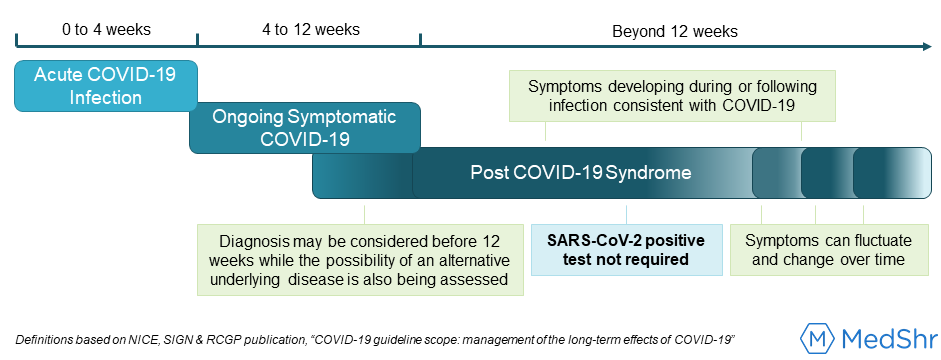
These uncertainties have made it challenging to clearly define the condition (or conditions) recognised by persisting signs and symptoms thought to be secondary to SARS-CoV-2 infection.[5] On 30th October 2020, the National Institute for Health and Clinical Excellence (NICE), the Scottish Intercollegiate Guidelines Network (SIGN), and the Royal College of General Practitioners (RCGP) released their guideline scope on management of the long-term effects of COVID-19 [6], and have assumed the terminology ‘post-COVID-19 syndrome’ with the following definition:
Significantly, this definition does not use ‘Long COVID’ in it’s nomenclature, a term which several authors have argued encapsulates the heterogeneity and uncertainty of this condition without limiting the reference by severity, chronicity or excluding the scope of patients affected.[3, 7, 8] However, given the increasing recognition that long-term effects from COVID-19 are not restricted to those who have been hospitalised with a severe form of the acute phase of infection [5], this definition clearly acknowledges that a positive SARS-CoV-2 test (either PCR, antigen or antibody) is not a requirement to diagnose post-COVID-19 syndrome (see figure 1).[6] Rather, it recognises a clinical diagnosis of an infection consistent with COVID-19 - which can be made retrospectively - and therefore is inclusive of patients who had to self-manage their illness at home often without access to a test.[9] It is also important to highlight a positive antibody test is not a prerequisite for diagnosis, given the variability and uncertainty in the expected levels of antibody titres following the acute phase of infection [10, 11], and the yet to be fully examined hypothesis that weaker immune responses may be a risk factor for the development of long-term COVID-19 symptoms.[2]
What do we know about Long-COVID thus far?
An accurate estimate of the prevalence of persisting symptoms from COVID-19 is not yet clear. An initial estimate from the COVID Symptom Study App, published on 6th June 2020, suggested one in ten patients using the app reported symptoms persisting for greater than three weeks.[12] A recent preprint article published on medRxiv (not yet peer-reviewed) from the same team revealed 13.3% of a sub-group of participants reported symptoms associated with COVID-19 for greater than 28 days, and 2.3% for more than 12 weeks.[13] Whilst this approach is providing valuable, rapidly available epidemiological data on long-term symptoms associated with COVID-19 [14], it is important to acknowledge a selection bias may be introduced by self-reporting of symptoms. Furthermore, the rates reported in this recent article are calculated after excluding patients who were asymptomatic, did not have a clear symptom onset, or who did not continue to regularly record symptoms on the app (overall a total of 84% of the identified PCR-confirmed cohort). However, other studies have reported even higher rates of persistent symptoms in both hospitalised patients [15, 16, 17] and non-hospitalised patients [17, 18, 17, 19]. Therefore, whilst a definitive prevalence is yet to be determined, it is clear that a significant proportion of patients infected with COVID-19 are suffering with debilitating, long-term effects which warrant urgent investigation.
Mechanisms and aetiological factors that underlie persistent symptoms from COVID-19 infection have been hypothesised but are not yet fully understood; the British Society of Immunology have created a useful rapid-review exploring some of these factors [20], and other authors are exploring hypotheses for possible mechanisms, for example the role of mast cells [21].
Significantly, the available literature from both patient-led research groups and scientific articles (both published and preprint) frequently highlight no discernible association between the severity of initial COVID-19 infection and the risk of persistent symptoms.[2, 17, 22] In a letter to the UK Health and Social Care Committee, the Long Covid Support Group emotively described, “...acquiring Coronavirus can lead to long term debilitating and distressing symptoms no matter your age, underlying health or fitness”.[9]
Data presented in two preprint articles suggest risk factors for Long COVID may include increasing age, increasing BMI, and/or being female [13], and also experiencing more symptoms earlier in the course of the infection (used as a proxy for severity in Ciruelli et al.).[13, 23]
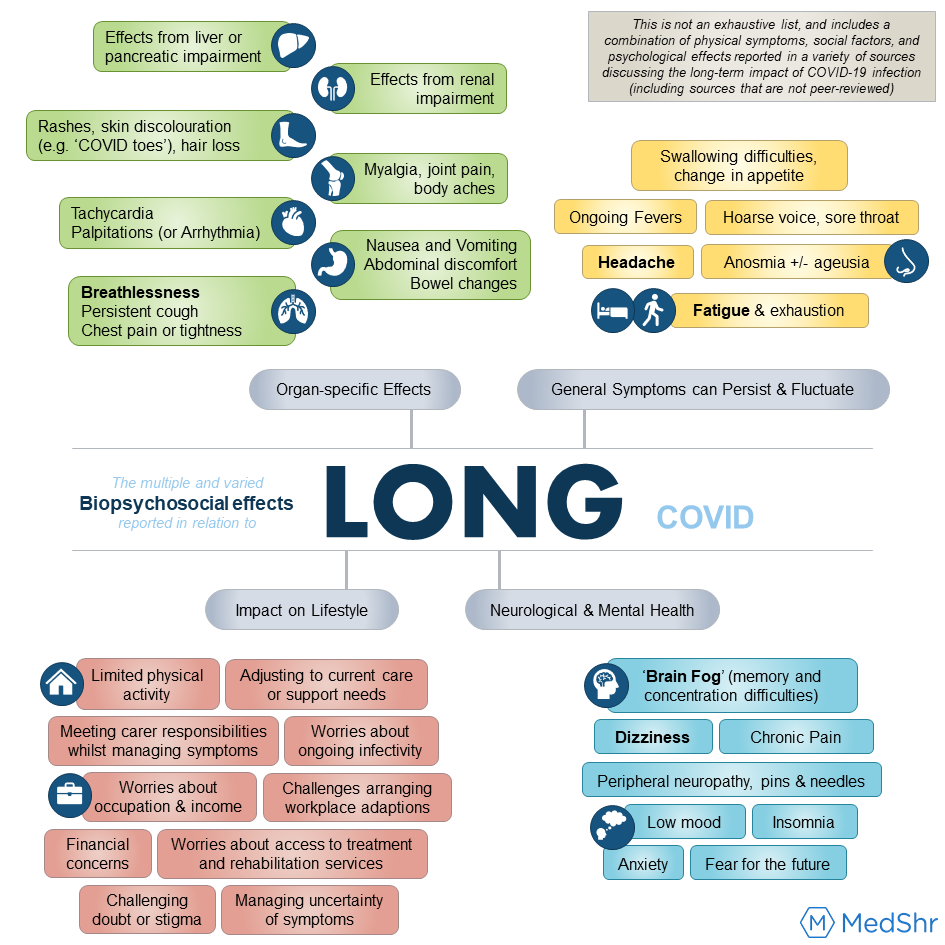
Symptoms of Long COVID vary markedly both for individual patients at different times of their illness, and in terms of the multiple body systems affected in different patients.[5, 22] A recent review by the National Institute of Health Research (NIHR) suggested that the multi-system and fluctuating symptoms experienced by patients may actually be due to multiple and interacting syndromes, such as Post-Intensive Care syndrome, Post-Viral Fatigue syndrome and Long-Term Covid syndrome.[5]
Figure 2 highlights a non-exhaustive list of some of the symptoms, social factors, and psychological effects commonly reported in the available literature exploring the long-term impact of COVID-19 infection (including sources that are not peer-reviewed).[5, 13, 22, 24, 25, 56] This figure is not intended to limit, define or categorise the subjective experience of this condition by patients, and there are recognised limitations to the biopsychosocial model; rather the hope is this provides an accessible summary which depicts the multiple, varied, and individualised effects this condition can have on patients, and therefore emphasise the need for a holistic approach to managing this condition.
What are the research challenges and questions to address?
From the available literature, several questions and challenges have been identified which must be addressed by future research studies into the long-term effects of COVID-19:
Establishing a working definition of Long COVID: as NICE suggests a working definition for long-term symptoms of COVID-19 as ‘post-COVID-19 syndrome’, it will be important to analyse how useful both patients and healthcare professionals find this as a working definition, and to be open to adapting this definition as required if new evidence emerges and our understanding of this syndrome increases. Equally, it is important to acknowledge that many patients with symptoms consistent with the working definition of ‘ongoing symptomatic COVID-19’ or ‘post-COVID-19 syndrome’ have expressed concern at the potential negative influence of current severity classifications for the acute illness phase which may lead to the misconception that any infection not resulting in respiratory compromise requiring hospitalisation is a mild case.[5] Involving patients in a discussion about what could be included in a functional grading scale for severity of living with COVID-19 will be essential [3, 26], and researchers should consider how this could be integrated with scoring or risk stratification tools for the acute phase of infection.[27] Critically, a working definition which is recognised internationally would allow for easier comparisons between different research studies.[28]
Identifying aetiological factors and how this translates to risk of developing Long COVID: increasing our understanding of the mechanisms which underlie COVID-19 infection is essential, with particular comparison of immunological and inflammatory responses between groups of patients with, 1) varying severity in the acute phase of infection and, 2) varying length of time to recovery or resolving symptoms.[28] If patterns can be established this may highlight risk factors which support epidemiological data for predicting groups of patients who may be at increased risk of Long COVID.[13] This would also help refine the definition of Long COVID, for example by identifying if subsets of syndromes with different predominant aetiologies exist [5], which in turn will help guide research and delivery of more focussed interventions. The possible association of persistent mild organ impairment, even in low-risk individuals (research from medRxiv, not yet peer-reviewed), with persisting symptoms of COVID-19 must also be fully explored.[29] In trying to understand the mechanisms which underlie Long COVID, calls have been made by leaders in the field of functional neurology to learn from the holistic research approaches utilised in this field which have led to several advances in understanding of these conditions.[30]
Optimising management and rehabilitation for Long COVID: in the next section, current management strategies for Long COVID, or post-COVID-19 syndrome, are addressed, and it will clearly be essential to design these services and evaluate their impact with significant input from patients with this condition.[5, 6] It will also be important to establish if there are any management strategies which, when employed in the acute phase of infection, can reduce progression to persisting COVID-19 symptoms.[28]
Consider the social and psychological implications of living with Long COVID: Future research must now consider the potential social and economical impact for patients who were previously employed but are temporarily (and possibly long-term) unable to work in the same role they had prior to COVID-19 infection.[5] This research would help shape support services and inform government policies to support this group of patients. Occupational health research must establish how to best accommodate for fluctuating absences amongst workforces [5], and a call has been made for the NHS to help lead the way as an adaptive and accommodating environment for employees returning to work who are suffering from symptoms of Long COVID.[9] It is also important that studies evaluating the long-term effects of COVID-19 assess the mental health effects of both acute infection and chronic symptoms. [31]
Yelin et al.[28] have suggested how these research studies could be designed, emphasising the need for multidisciplinary, multicentre, international studies. Several research studies have been launched, and are summarised in the NIHR themed review.[5] These studies aim to examine a range of patient cohorts, including:
Hospitalised Patients: PHOSP-COVID (including analysis of the impact of hospital treatments on long-term effects)
Both hospitalised and non-hospitalised patients, but requiring a positive SARS-CoV-2 test for inclusion: Long-term Impact of Infection With Novel Coronavirus (LIINC), and focusing on organ health through imaging follow-up, the COVERSCAN study
Patients not immediately requiring hospitalisation: International SARS-CoV-2 Infection Observational Study (ICOS)
Inclusion of all patients with either laboratory or clinical diagnosis of COVID-19: ISARIC Global COVID-19 Long term follow up study
Prospective, including participants both with and without COVID-19, to evaluate factors which determine risk, severity and recovery from COVID-19: COVIDENCE UK Study
In addition, international projects such as the COVID Symptom Study App and the Patient Led Research surveys previously mentioned, are also helping shape our understanding of Long COVID, and issues highlighted by early patient-led research has been recognised recently in a meeting with the WHO.[32] However, as with all good scientific research, it is important to ensure that study results are interpreted with reference to the study population; some challenges which should be considered with the data collected in these projects include:
Selection bias may be introduced from having a self-selecting sample; equally a degree of recall bias may be introduced.
For certain methods of data collection, e.g. smartphone apps or social media groups, participation bias could be introduced by patients at the extremes of age or with decreased ability to use these methods (e.g. children or care home residents) being unable to contribute to the results; similarly some underrepresented patient groups in medical research (e.g. homeless patients) may not have access to these technologies.[5]
It is also important to consider if participation bias may be introduced if patients who have recovered from COVID-19 are then less likely to continue to contribute to these data collecting methods.
Indeed, results reported from these studies highlight these issues within their publications. This should not negate the validity or value of results from these studies, but rather highlight that future research must also ensure patients from groups which may be underrepresented are included in studies exploring the long-term effects of COVID-19.[3, 5] Authors have already raised this issue, for example highlighting the importance of examining the impacts of Long COVID in paediatric patients.[33, 34]
What Support is available for patients with Long COVID?
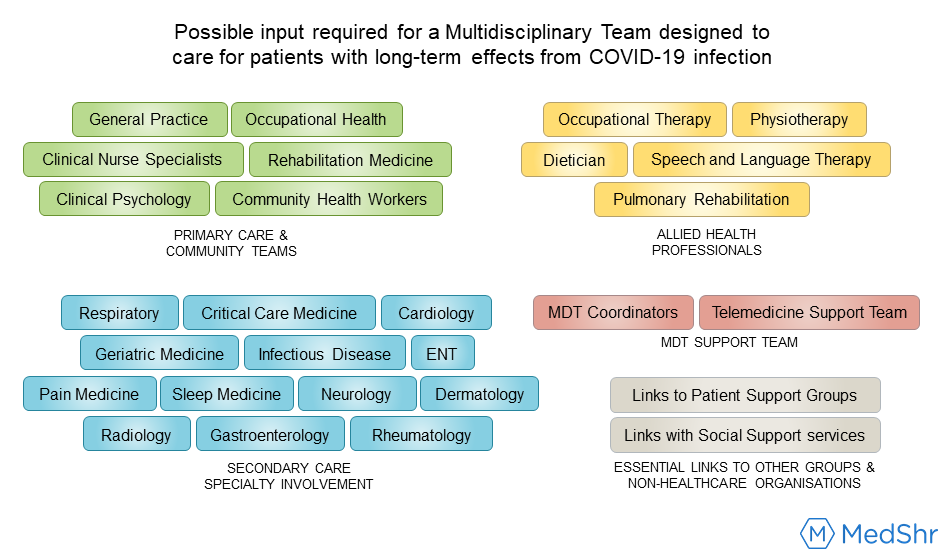
Given the fluctuating severity and multi-system effects associated with Long COVID, it is unsurprising that both patient support groups and researchers have emphasised that services created to manage the effects of this condition must have a holistic, multidisciplinary approach.[5, 35, 36]
The NHS launched the ‘Your COVID Recovery’ website hub earlier this year, and in October committed to establishing a ‘NHS England Long Covid taskforce’, which critically will also include patients with Long COVID.[37] Furthermore, multidisciplinary clinics dedicated to Long COVID are planned across the UK, where patients will be able to access support for physical, cognitive and psychological effects from their condition.[34, 37] It will be important to design services that meet the rehabilitation needs of both hospitalised and non-hospitalised patients [19, 36], and whilst specialist secondary care clinics will play a central role, the importance of integrating these services with COVID-19 support teams in primary care and the community will also be essential.[38] Sivan et al. [38] have published guidance on how such an integrated rehabilitation pathway may be structured, and figure 3 demonstrates the scale of the specialised MDT which could be required to deliver these services.[34]
Authors have proposed using telemedicine both for screening and delivering certain management options to try and ensure patients are able to access targeted services specific to their needs in a timely manner.[39] Similarly, novel approaches described in preprint articles such as the ABCoV-tool [40] and the COVID Symptoms Study App [13] could provide unique insight into monitoring individual disease burden and therefore directing services to patients as required.
In addition to launching these specialist hospital and community services, patient-led support groups have also called for formalised funding as recognition of the important role these groups have in supporting recovery.[9] Furthermore, in recognition of the significant mental health impact that COVID-19 - both as a direct consequence of infection or as an indirect impact from the global pandemic - may have on patients, adequate funding for mental health services will be an essential component of public health strategies going forward.[31, 41, 42] As discussed above, ensuring that there is also appropriate occupational health advocacy for patients with Long COVID to enable a supportive and adaptive return to work where possible is important.[5, 9]
How can Healthcare Professionals keep up-to-date with this guidance?
One striking feature of the recent NIHR report which has also been echoed by patient support groups [9, 22], is the description of patients with Long COVID feeling like their symptoms were being doubted.[5] Qualitative research examining this emphasised the perceived therapeutic value for patients in having healthcare professionals (specifically their GP in this study) simply acknowledge and believe their symptoms, even if the optimal management going forward is not immediately clear.[43] A key challenge for the healthcare profession now is ensuring that not only is guidance for the best-evidenced management of SARS-CoV-2 in the acute phase widely available, but also that accessible, evidence-based resources are available to empower healthcare professionals to provide accurate, consistent and realistic information to patients with long-term effects of COVID-19.[2, 5] Therefore, as emphasised by the NICE guideline scope [6], it will be important that the ‘lived experiences’ of patients are incorporated into developing clinical guidelines.
Follow-up guidance for individual specialities and conditions is emerging, for example respiratory follow-up for patients with COVID-19 pneumonia [44], and considerations for managing chronic pain after COVID-19 [45]. Consensus statements from rehabilitation experts have also been produced for COVID-19 rehabilitation [46], and the NIHR living review is running webinars on a range of topics related to long COVID.[5] However, it will be important that new guidelines also provide approaches for supporting recovery and rehabilitation for patients who managed their symptoms at home and therefore may not have had documented evidence of clinical infection.[36, 38]
A key role for healthcare teams managing patients with suspected Long COVID will be ensuring that symptoms are appropriately investigated to exclude other causes before being attributed solely to SARS-CoV-2 infection.[2, 5] Such approach was highlighted in the NIHR report and has been emphasised in the definitions laid out in the NICE, SIGN and RCGP scope guidance.[6]
Challenges for Managing Long COVID in Low- and Middle-Income Countries (LMICs)
At the time of writing, there was no published literature that we could identify discussing the potential challenges of caring for patients with long COVID in low- and middle-income countries (LMICs).
Given the potential burden of Long COVID globally, and previously identified gaps in the provision of rehabilitation services to patients living with a disability in some LMICs [47], it is essential for research to address this global need to help inform policies and guide healthcare professionals. Importantly, research into the long-term effects of COVID-19 must also consider the potential challenges patients face which are unique to their region, culture or society, as the burden of the condition is influenced by each individual's unique circumstances.[5, 48]
Examples of some specific challenges that research into the effects of Long COVID in LMICs may need to consider and address include:
Weak primary health care services: this was identified by the WHO as one of the greatest threats to global health in 2019 [49], and this could prove a significant challenge as primary care is likely to play a central role in providing recovery and rehabilitation services for patients with Long COVID. However, where services may need to be delivered in the context of ongoing social distancing, the potential strengths in healthcare systems built on strong networks of community health workers who can help deliver long COVID therapies to patients in their own homes should not be underestimated.[50]
Barriers to accessing Long COVID clinics: including challenges travelling to clinics and financial barriers in paying for access to these services.[51] Barriers could also be created by inadequate infrastructure to support follow-up and screening (e.g. by telephone) to detect patients with possible long-term effects from COVID-19.
Role of Telemedicine: several authors have proposed utilising telemedicine solutions for providing rehabilitation services for patients with Long COVID, but this will be dependent on the patient’s ability to access and use the technology required to enable this approach. Positively, there are reports of successful use of smartphone-based telemedicine programmes for delivering mental health services which predate the COVID-19 pandemic, and news reports suggest these have proved vital in trying to preserve and boost essential mental health services during this time.[52]
Access to a Long COVID MDT: restricted access to specialist members of the proposed Long COVID multidisciplinary team, for example physiotherapists [53], could prove challenging in low-resource regions.
This is by no means an exhaustive list, and moving forward the importance of the global healthcare community advocating that appropriate attention is drawn to addressing the long-term effects of COVID-19 for all patients is essential.[54] These needs must be met alongside the unprecedented and ongoing challenges of controlling the spread of COVID-19 and optimising care in the acute phase of the infection. Moving forward, an integrated approach to research and the design of management and rehabilitation services which includes patients, scientists, healthcare professionals, and policy makers together in the discussion is likely to be key.[55]
Useful Resources:
Below is a list of some resources related to the long-term effects of COVID-19 which readers may find useful, with several of these resources including their own resource banks. Although divided into resources for healthcare professionals and patients, as discussed above, healthcare professionals may also find several of the resources created by the patient support groups beneficial in increasing their awareness of this evolving condition. If you feel a useful resource is missing please feel free to share the details for this in the comments section below this article.
Emerging Guidance and eLearning for Healthcare Professionals:
NIHR: Living with Covid19 - Themed Review and a webinar on this topic
Asthma UK and British Lung Foundation: Post-COVID Hub
eLearning for Health, Health Education England: COVID-19 Recovery and Rehabilitation
RCGP eLearning: Recovery for COVID-19
Patient Safety Learning (The Hub): Clear NHS plan needed to reassure Long COVID patients
Support Groups and Information for Patients:
NHS: Your COVID Recovery
Asthma UK and British Lung Foundation: Post-COVID Hub (Support)
Patient Support Groups - a collection of some of the groups helping connect COVID-19 survivors and support research into the long-term effects of this infection:
Continue the Discussion:
Join the COVID-19 discussion groups for healthcare professionals on MedShr:




References:
[1] Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020 May;20(5):533-534. doi: 10.1016/S1473-3099(20)30120-1. Epub 2020 Feb 19. Erratum in: Lancet Infect Dis. 2020 Sep;20(9):e215. PMID: 32087114; PMCID: PMC7159018.
[2] Greenhalgh T, Knight M, A'Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. BMJ. 2020 Aug 11;370:m3026. doi: 10.1136/bmj.m3026. PMID: 32784198.
[3] Callard F, Perego E. How and why patients made Long Covid. Soc Sci Med, 2020; [in press]; 113426, ISSN 0277-9536. DOI: 10.1016/j.socscimed.2020.113426
[4] Ahmed H, Patel K, Greenwood DC, Halpin S, Lewthwaite P, Salawu A, Eyre L, Breen A, O'Connor R, Jones A, Sivan M. Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: A systematic review and meta-analysis. J Rehabil Med. 2020 May 31;52(5):jrm00063. doi: 10.2340/16501977-2694. PMID: 32449782.
[5] National Institute for Health Research. Themed Review - Living with Covid19. 2020 Oct 15. DOI: 10.3310/themedreview_41169
[6] National Institute for Health and Clinical Excellence (NICE), Scottish Intercollegiate Guidelines Network (SIGN), Royal College of General Practitioners (RCGP). COVID-19 guideline scope: management of the long-term effects of COVID-19. [GID-NG10179]. 2020 Oct 30. Available at: https://www.nice.org.uk/guidance/indevelopment/gid-ng10179
[7] Perego E, Callard F, Stras L, Melville-Jóhannesson B, Pope R, Alwan NA. Why we need to keep using the patient made term “Long Covid” [Internet]. BMJ Opinion Blog. Published 2020 Oct 1. Available at: https://blogs.bmj.com/bmj/2020/10/01/why-we-need-to-keep-using-the-patient-made-term-long-covid/
[8] Ondine Sherwood O. Why 'Post Covid-19 Syndrome' is the wrong choice of name [Internet]. LongCovidSOS. 2020 Nov 16. Available at: https://www.longcovidsos.org/
[9] Long Covid Support Group. Public letter to: Rt Hon Jeremy Hunt, Chair, UK Health and Social Care Committee. 2020 Aug 28. Available at: www.longcovid.org/
[10] Gudbjartsson DF, Norddahl GL, Melsted P, et al. Humoral Immune Response to SARS-CoV-2 in Iceland. N Engl J Med. 2020 Oct 29;383(18):1724-1734. doi: 10.1056/NEJMoa2026116. Epub 2020 Sep 1. PMID: 32871063; PMCID: PMC7494247.
[11] Ward W, Cooke C, Atchison C, et al. Declining prevalence of antibody positivity to SARS-CoV-2: a community study of 365,000 adults. medRxiv 2020 Oct 27 [preprint].10.26.20219725; doi: https://doi.org/10.1101/2020.10.26.20219725
[12] COVID Symptom Study. How long does COVID-19 last? [internet]. 2020 Jun 6. Available at: https://covid.joinzoe.com/post/covid-long-term
[13] Sudre CH, Murray B, Varsavsky T, et al. Attributes and predictors of Long-COVID: analysis of COVID cases and their symptoms collected by the Covid Symptoms Study App. medRxiv. 2020 Oct 27 [preprint]; 10.19.20214494; doi: 10.1101/2020.10.19.20214494
[14] Drew DA, Nguyen LH, Steves CJ, Menni C, Freydin M, Varsavsky T, Sudre CH, Cardoso MJ, Ourselin S, Wolf J, Spector TD, Chan AT; COPE Consortium. Rapid implementation of mobile technology for real-time epidemiology of COVID-19. Science. 2020 Jun 19;368(6497):1362-1367. doi: 10.1126/science.abc0473. Epub 2020 May 5. PMID: 32371477; PMCID: PMC7200009.
[15] Carfì A, Bernabei R, Landi F; Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19. JAMA. 2020 Aug 11;324(6):603-605. doi: 10.1001/jama.2020.12603. PMID: 32644129; PMCID: PMC7349096.
[16] Arnold DT, Hamilton FW, Milne A, et al. Patient outcomes after hospitalisation with COVID-19 and implications for follow-up; results from a prospective UK cohort. medRxiv. 2020 Aug 14 [preprint]; 08.12.20173526; doi: 10.1101/2020.08.12.20173526
[17] Townsend L, Dyer AH, Jones K, et al. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. medRxiv. 2020 Jul 30 [preprint]; 07.29.20164293; doi: 10.1101/2020.07.29.20164293
[18] Tenforde MW, Kim SS, Lindsell CJ, et al. Symptom Duration and Risk Factors for Delayed Return to Usual Health Among Outpatients with COVID-19 in a Multistate Health Care Systems Network - United States, March-June 2020. MMWR Morb Mortal Wkly Rep. 2020 Jul 31;69(30):993-998. doi: 10.15585/mmwr.mm6930e1. PMID: 32730238; PMCID: PMC7392393.
[19] Vaes AW, Machado FVC, Meys R, Delbressine JM, Goertz YMJ, Van Herck M, Houben-Wilke S, Franssen FME, Vijlbrief H, Spies Y, Van 't Hul AJ, Burtin C, Janssen DJA, Spruit MA. Care Dependency in Non-Hospitalized Patients with COVID-19. J Clin Med. 2020 Sep 12;9(9):2946. doi: 10.3390/jcm9092946. PMID: 32932582; PMCID: PMC7564703.
[20] British Society for Immunology. Long-term immunological health consequences of COVID-19. London. 2020 Aug 13. Available at: www.immunology.org
[21] Afrin LB, Weinstock LB, Molderings GJ. Covid-19 hyperinflammation and post-Covid-19 illness may be rooted in mast cell activation syndrome. Int J Infect Dis. 2020 Sep 10;100:327-332. doi: 10.1016/j.ijid.2020.09.016. Epub ahead of print. PMID: 32920235; PMCID: PMC7529115.
[22] Assaf G, Davis H, McCorkell L, et al. An analysis of the prolonged COVID-19 symptoms survey by Patient-Led Research Team. Patient Led Research. 2020 May 11; available ar: https://patientresearchcovid19.com/
[23] Cirulli ET, Schiabor Barrett KM, Riffle S, et al. Long-term COVID-19 symptoms in a large unselected population. medRxiv. 2020 Oct 24 [preprint]. 10.07.20208702; doi: 10.1101/2020.10.07.20208702
[24] Royal College of General Practitioners. Management of the long term effects of COVID-19: The RCGP response and top tips for caring for our patients. RCGP; 2020 Oct 30 (V1). Available at: https://elearning.rcgp.org.uk/
[25] Tony Blair Institute for Global Health. Long Covid: Reviewing the Science and Assessing the Risk. Published 2020 Oct 5.
[26] Lokugamage AU, Taylor S, Rayner C. Patients’ experiences of “longcovid” are missing from the NHS narrative [internet]. BMJ Opinion Blog. Published 2020 Jul 10. Available at: https://blogs.bmj.com/bmj/2020/07/10/patients-experiences-of-longcovid-are-missing-from-the-nhs-narrative/
[27] Klok FA, Boon GJAM, Barco S, Endres M, Geelhoed JJM, Knauss S, Rezek SA, Spruit MA, Vehreschild J, Siegerink B. The Post-COVID-19 Functional Status scale: a tool to measure functional status over time after COVID-19. Eur Respir J. 2020 Jul 2;56(1):2001494. doi: 10.1183/13993003.01494-2020. PMID: 32398306; PMCID: PMC7236834.
[28] Yelin D, Wirtheim E, Vetter P, Kalil AC, Bruchfeld J, Runold M, Guaraldi G, Mussini C, Gudiol C, Pujol M, Bandera A, Scudeller L, Paul M, Kaiser L, Leibovici L. Long-term consequences of COVID-19: research needs. Lancet Infect Dis. 2020 Oct;20(10):1115-1117. doi: 10.1016/S1473-3099(20)30701-5. Epub 2020 Sep 1. PMID: 32888409; PMCID: PMC7462626.
[29] Dennis A, Wamil M, Kapur S, et al. Multi-organ impairment in low-risk individuals with long COVID. medRxiv. 2020 Oct 16.10.14.20212555; doi: 10.1101/2020.10.14.20212555
[30] Stone J, Carson A. Reader response: Long-Haul COVID. Published 2020 Sep 29. Comment in: Nath A. Long-Haul COVID. Neurology. 2020 Sep 29;95(13):559-560. doi: 10.1212/WNL.0000000000010640. Epub 2020 Aug 11. PMID: 32788251.
[31] Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2020 Nov 9:S2215-0366(20)30462-4. doi: 10.1016/S2215-0366(20)30462-4. Epub ahead of print. Erratum in: Lancet Psychiatry. 2020 Nov 12;: PMID: 33181098.
[32] Lokugamage A, Rayner C, Simpson F, Carayon L. We have heard your message about long covid and we will act, says WHO [internet]. BMJ Opinion Blog. Published 2020 Sep 3. Available at: https://blogs.bmj.com/bmj/2020/09/03/we-have-heard-your-message-about-long-covid-and-we-will-act-says-who/
[33] Simpson F, Lokugamage A. Counting long covid in children [internet]. BMJ Opinion Blog. Published 2020 Oct 16. Available at: https://blogs.bmj.com/bmj/2020/10/16/counting-long-covid-in-children/
[34] National Health Service. National Guidance for post-COVID syndrome assessment clinics. 2020 Nov 6; reference: 001599. Available at: https://www.england.nhs.uk/coronavirus/publication/national-guidance-for-post-covid-syndrome-assessment-clinics/
[35] Sheehy LM. Considerations for Postacute Rehabilitation for Survivors of COVID-19. JMIR Public Health Surveill. 2020 May 8;6(2):e19462. doi: 10.2196/19462. PMID: 32369030; PMCID: PMC7212817.
[36] Halpin SJ, McIvor C, Whyatt G, Adams A, Harvey O, McLean L, Walshaw C, Kemp S, Corrado J, Singh R, Collins T, O'Connor RJ, Sivan M. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation. J Med Virol. 2020 Jul 30. doi: 10.1002/jmv.26368. Epub ahead of print. PMID: 32729939.
[37] National Health Service. NHS to offer ‘long covid’ sufferers help at specialist centres [Internet]. NHS; 2020 Oct 7. Available at: https://www.england.nhs.uk/2020/10/nhs-to-offer-long-covid-help/
[38] Sivan M, Halpin S, Hollingworth L, Snook N, Hickman K, Clifton IJ. Development of an integrated rehabilitation pathway for individuals recovering from COVID-19 in the community. J Rehabil Med. 2020 Aug 24;52(8):jrm00089. doi: 10.2340/16501977-2727. PMID: 32830284.
[39] Salawu A, Green A, Crooks MG, Brixey N, Ross DH, Sivan M. A Proposal for Multidisciplinary Tele-Rehabilitation in the Assessment and Rehabilitation of COVID-19 Survivors. Int J Environ Res Public Health. 2020 Jul 7;17(13):4890. doi: 10.3390/ijerph17134890. PMID: 32645876; PMCID: PMC7369849.
[40] Noort EMV, Claessens D, Moor CC, Berg CVD, Kasteleyn M, Veen HCI', Schayck OV, Chavannes NH. Online Assessment of the Burden of COVID-19: the ABCoV-tool. JMIR Preprints. 17/07/2020:22603. DOI: 10.2196/preprints.22603
[41] National Institute for Health Research. Mental health and COVID-19 [online]. NIHR; 2020 Sep 2. Available at: https://doi.org/10.3310/collection_40756
[42] Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav Immun. 2020 Oct;89:531-542. doi: 10.1016/j.bbi.2020.05.048. Epub 2020 May 30. PMID: 32485289; PMCID: PMC7260522.
[43] Kingstone T, Taylor AK, O'Donnell CA, Atherton H, Blane DN, Chew-Graham CA. Finding the 'right' GP: a qualitative study of the experiences of people with long-COVID. BJGP Open. 2020 Oct 13:bjgpopen20X101143. doi: 10.3399/bjgpopen20X101143. Epub ahead of print. PMID: 33051223.
[44] George PM, Barratt SL, Condliffe R, Desai SR, Devaraj A, Forrest I, Gibbons MA, Hart N, Jenkins RG, McAuley DF, Patel BV, Thwaite E, Spencer LG. Respiratory follow-up of patients with COVID-19 pneumonia. Thorax. 2020 Nov;75(11):1009-1016. doi: 10.1136/thoraxjnl-2020-215314. Epub 2020 Aug 24. PMID: 32839287; PMCID: PMC7447111.
[45] Kemp HI, Corner E, Colvin LA. Chronic pain after COVID-19: implications for rehabilitation. Br J Anaesth. 2020 Oct;125(4):436-440. doi: 10.1016/j.bja.2020.05.021. Epub 2020 May 31. PMID: 32560913; PMCID: PMC7261464.
[46] Barker-Davies RM, O'Sullivan O, Senaratne KPP, Baker P, Cranley M, Dharm-Datta S, Ellis H, Goodall D, Gough M, Lewis S, Norman J, Papadopoulou T, Roscoe D, Sherwood D, Turner P, Walker T, Mistlin A, Phillip R, Nicol AM, Bennett AN, Bahadur S. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med. 2020 Aug;54(16):949-959. doi: 10.1136/bjsports-2020-102596. Epub 2020 May 31. PMID: 32475821; PMCID: PMC7418628.
[47] World Health Organization. (2015). WHO global disability action plan 2014-2021: better health for all people with disability. World Health Organization. https://apps.who.int/iris/handle/10665/199544
[48] Ladds E, Rushforth A, Wieringa S, Taylor S, Rayner C, Husain L, Greenhalgh T. Persistent symptoms after Covid-19: qualitative study of 114 “long Covid” patients and draft quality criteria for services [preprint]. medRxiv 2020.10.13.20211854; doi: 10.1101/2020.10.13.20211854
[49] World Health Organization. Ten threats to global health in 2019 [online]. Available at: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019
[50] World Health Organization. Easing COVID-19 impact on key health services [online]. Available from: https://www.afro.who.int/news/easing-covid-19-impact-key-health-services
[51] Shadmi E, Chen Y, Dourado I, Faran-Perach I, Furler J, Hangoma P, Hanvoravongchai P, Obando C, Petrosyan V, Rao KD, Ruano AL, Shi L, de Souza LE, Spitzer-Shohat S, Sturgiss E, Suphanchaimat R, Uribe MV, Willems S. Health equity and COVID-19: global perspectives. Int J Equity Health. 2020 Jun 26;19(1):104. doi: 10.1186/s12939-020-01218-z. PMID: 32586388; PMCID: PMC7316580.
[52] Adepoju P. Africa turns to telemedicine to close mental health gap. Lancet Digit Health. 2020 Nov;2(11):e571-e572. doi: 10.1016/S2589-7500(20)30252-1. Epub 2020 Oct 19. PMID: 33103096; PMCID: PMC7571965.
[53] Abdullahi A, Bello B, Mukhtar NB, Kaka B, Abba MA, Usman JS, Shittu A, Mayana KI, Maiwada SA, Mohammed J. Physiotherapy management of COVID-19 in Africa: Ongoing efforts, challenges, and future directions. Physiother Theory Pract. 2020 Aug;36(8):871-872. doi: 10.1080/09593985.2020.1798163. Epub 2020 Jul 29. PMID: 32723204.
[54] Brown DA, O'Brien KK, Josh J, Nixon SA, Hanass-Hancock J, Galantino M, Myezwa H, Fillipas S, Bergin C, Baxter L, Binette M, Chetty V, Cobbing S, Corbett C, Ibanez-Carrasco F, Kietrys D, Roos R, Solomon P, Harding R. Six Lessons for COVID-19 Rehabilitation From HIV Rehabilitation. Phys Ther. 2020 Oct 30;100(11):1906-1909. doi: 10.1093/ptj/pzaa142. PMID: 32737967; PMCID: PMC7454859.
[55] Lutchmansingh DD, Knauert MP, Antin-Ozerkis DE, Chupp G, Cohn L, Dela Cruz CS, Ferrante LE, Herzog EL, Koff J, Rochester CL, Ryu C, Singh I, Tickoo M, Winks V, Gulati M, Possick JD. A clinic blueprint for post-COVID-19 RECOVERY: Learning from the past, looking to the future. Chest. 2020 Nov 4:S0012-3692(20)35125-4. doi: 10.1016/j.chest.2020.10.067. Epub ahead of print. PMID: 33159907; PMCID: PMC7641526.
[56] Del Rio C, Collins LF, Malani P. Long-term Health Consequences of COVID-19. JAMA. 2020 Oct 5. doi: 10.1001/jama.2020.19719. Epub ahead of print. PMID: 33031513.
Article by Dr Ryan Broll, MedShr Open Editorial Team, Medical Education Fellow
Loading Author...
Sign in or Register to comment