Contact Tracing in COVID-19
This page summarises relevant WHO guidance on contact tracing for educational purposes. Visit links below for full guidance.
Why contact trace?
to the break human-to-human transmission sequence which spreads SARS-CoV-2
to maintain the reproduction number <1
Requirements for effective contact tracing:
systematically applied
involves community engagement
adequate testing capacity
a skilled trained workforce
How is contact tracing applied in different transmission-scenarios?
Where there are no cases, efforts should focus on developing contact tracing capacity
Where there are sporadic cases contact tracing is vital
Where there are clusters of cases contact tracing can reduce or stop transmission
Where community transmission is widespread, contact tracing may have to focus on high risk facilities (e.g. institutions, care homes, prisons) and healthcare workers. Extensive contact tracing should take place as much as is possible.
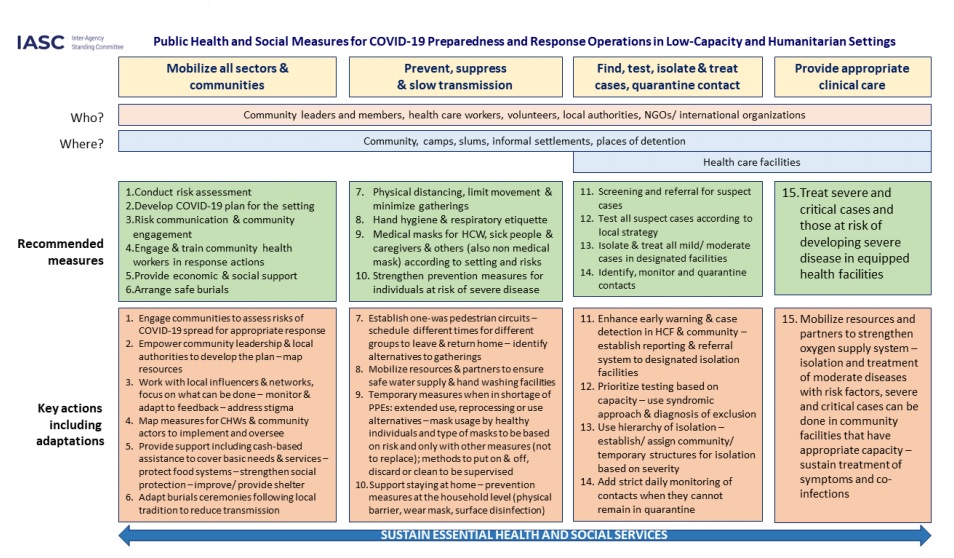
This table from the IASC summarises the required elements for responding to COVID-19 in low capacity settings, including approaches to contact tracing:
What counts as a contact?

*Tip: Contact tracing is the same for all COVID-19 positive cases regardless of whether they symptomatic or not.*
What counts s a contact continued
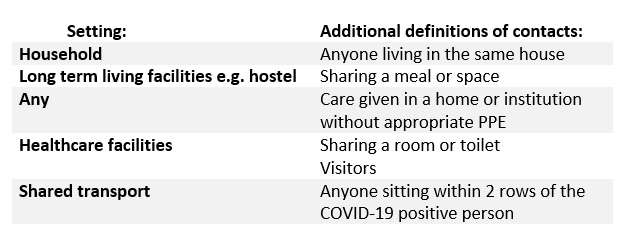
There are some additional definitions which depend on individual settings:
How to identify and consult contacts?
Requires interview of the patient and or caregivers
What information will you seek from contacts?
· Confirm the contact meets definition
· Whether they are experiencing any symptoms
What information will you share with contacts?
· What contact tracing is and why it is being done
· How and where they should quarantine
· How their information will be used and kept
· Symptoms to monitor for
· What to do if they become sick
How are contacts followed-up?
Contacts should be monitored every day for 14 days after their contact with a COVID-19 positive person. Monitoring may take the form of:
Direct consultation
Telephone or remote consultation
Self-reporting even if well through online forms
Summary:
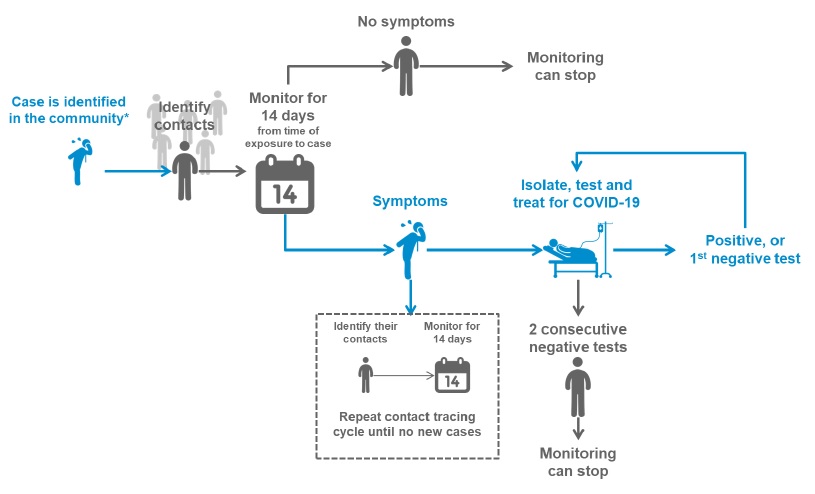
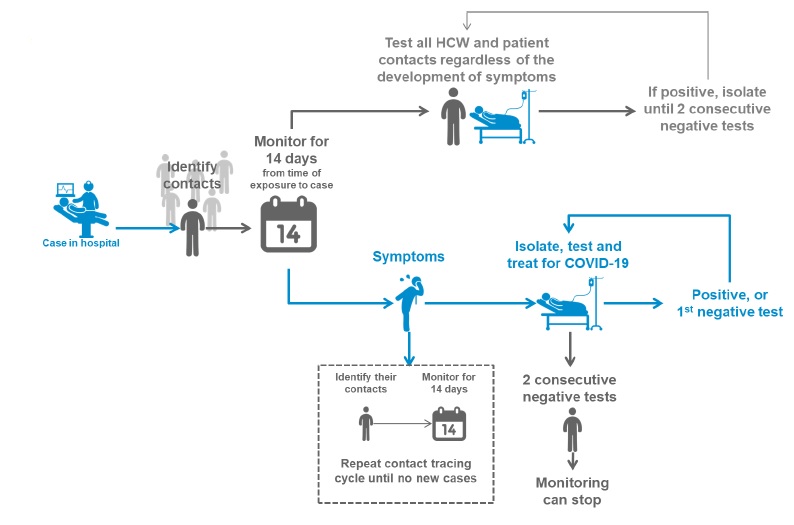
These useful info-graphics from WHO summarise the contact tracing process in the community and healthcare settings.
Community contact tracing:
Healthcare contact tracing:
References:
World Health Organization. Considerations in the investigation of cases and clusters of COVID-19, Interim guidance. 2 April 2020. [Online]. Available from: https://www.who.int/publications-detail/considerations-in-the-investigation-of-cases-and-clusters-of-covid-19 [Accessed 1.6.20]
World Health Organization. Contact tracing in the context of COVID-19. 10 May 2020. [Online] Available from: https://www.who.int/publications-detail/contact-tracing-in-the-context-of-covid-19 [Accessed 1.6.20].
Inter-Agency Standing Committee. Public Health and Social Measures for COVID-19 preparedness and response in Low Capacity and Humanitarian Settings. May 2020. [Online]. Available from: https://interagencystandingcommittee.org/system/files/2020-05/IASC%20Interim%20Guidance%20on%20Public%20Health%20and%20Social%20Measures%20for%20COVID-19%20Preparedness%20and%20Response%20Operations%20in%20Low%20Capacity%20and%20Humanitarian%20Settings.pdf [Accessed 1.6.20].
Written by Dr Rachel Coles, education fellow, 1st June 2020.
Loading Author...
Sign in or Register to comment