Difficult decisions: ethical healthcare resource allocation
“There is no way to find an exception, we have to decide who must die and whom we shall keep alive.” (1)
This stark message came from colleagues in Italy at the height of their initial COVID-19 peak, as healthcare professionals sought to share information from the front lines and help other healthcare systems prepare for when novel Coronavirus hit.
The present outbreak has resulted in unprecedented resource shortages, particularly in European countries whose populations, clinicians and healthcare systems had not previously had to accept resource scarcity to this degree. As the pandemic develops globally, it has affected a wider range of countries, including those more familiar with management of infectious disease outbreaks and navigation of resource allocation. In the context of this global pandemic, how can ethics guide the healthcare response to novel Coronavirus?
This article summarises key concepts from published works on ethical resource allocation in the COVID-19 outbreak of relevance to clinicians.
Establishing the landscape:
-Authors caution that the decision to set limits is not optional (2)
-There is a need to do so pro-actively, ethically and consistently (2)
-Decision-makers must accept that imposition of resource rationing is likely to be criticised and met with backlash, and that there will always be ethical complication in every framework (1)
-However, the ethical ramifications are likely to be worse if left unaddressed and left to unfold without guidance (1)
-There is an emotional toll on clinicians shouldering responsibility for allocating scarce resource as individuals, which could be mitigated by overarching guidance and practical approaches (1,2,3,4)
-In a pandemic, there is an ethical strain whereby the duty of healthcare professionals must shift to a greater extent from responsibility to individuals to responsibility to the whole community (3)
Principles:
Maximising benefit to all
The overarching principle agreed on by all papers was that available resources should be used in a manner which allows as many lives as possible to be saved.
Saving as many life years as possible:
1. Prioritisation of those most likely to survive the acute event
2. Prioritisation of the most likely to live longest after treatment
This requires assessment of short-term survival likelihood e.g. by using Sequential Organ Failure Assessment (SOFA) score and prognostication of long term survival, taking account of co-morbidity and age (2). A major ethical criticism of such approaches would be ageism.
These decisions are taken every day by physicians around the world not only in relation to intubation and ventilation for intensive care, but also for surgery, coronary interventions and cancer therapy. The coronavirus pandemic has brought this into stark focus in view of the unprecedented numbers of patients with respiratory compromise who may need intubation and ventilation.
Saving life-savers:
- Authors argue ‘instrumental value’ must be taken into account, meaning giving priority to those who can go on to save others if they survive, or who have saved others previously. Prioritising front-line health-care workers may have ethical basis by benefiting the overall population (2,3).
- Research participation by patients to benefit future patients should be considered and rewarded (2)
Equal treatment
Some authors sited the inherent inequality in a ‘first-come first-served’ model of allocation, which could for example be bias against people who observed public health measures or live furthest from hospitals (2). They propose imposed random-selection would improve fairness and transparency whilst being quick, such as via a lottery system (2). This theortical approach, however fair it may seen, is at odds with the well-established principles of providing treatment in relation to clinical need.
Additionally, throughout the outbreak it is proposed that patients be allocated resources using the same approach regardless of whether they are presenting with COVID-19 or another illness (2).
Prioritisation of those with most to gain
This argument proposes that younger people who will have lived the shortest lives if they die untreated have the most to gain from treatment and should be prioritised for acute respiratory support or live saving therapy (2). This is also in keeping with existing data that show younger people are more likely to tolerate ventilation, leading to recovery and longer term survival.
Similarly healthcare professionals, the elderly and at-risk groups should be prioritised for vaccines as they would have most to gain as a group by not contracting COVID-19 (2).
Open communication
Authors report there should be transparency about what guiding principles are being used to allocate resources and how these decisions have been made (4). There should be open communication about resource allocation to promote awareness and trust.
Practical approaches:
With these principles in mind, some practical approaches have been suggested to implement an ethical approach to resource allocation:
-Development of prioritisation guidelines to attempt to standardise the approach (2)
-Separation of resource allocation from clinical care using ‘triage officers / teams / committees’ who make resource decisions and communicate these (1,4). This approach hopes to mitigate emotional impacts on clinicians, as well as allowing clinicians to maintain responsibility to individual patients (4). This approach is now in practiced in a number of UK hospitals to sense check and review policy decisions.
-Central review of the resource allocation process nationally to ensure inequities are minimised (1)
-Regular review of resource allocation frameworks to ensure they evolve with disease knowledge (1)
-Drive an increase in patients documenting advanced care directives (2)
-Provide information to relatives at admission about resource allocation procedures and principles, including that resources may be required for someone else under set circumstances (2)
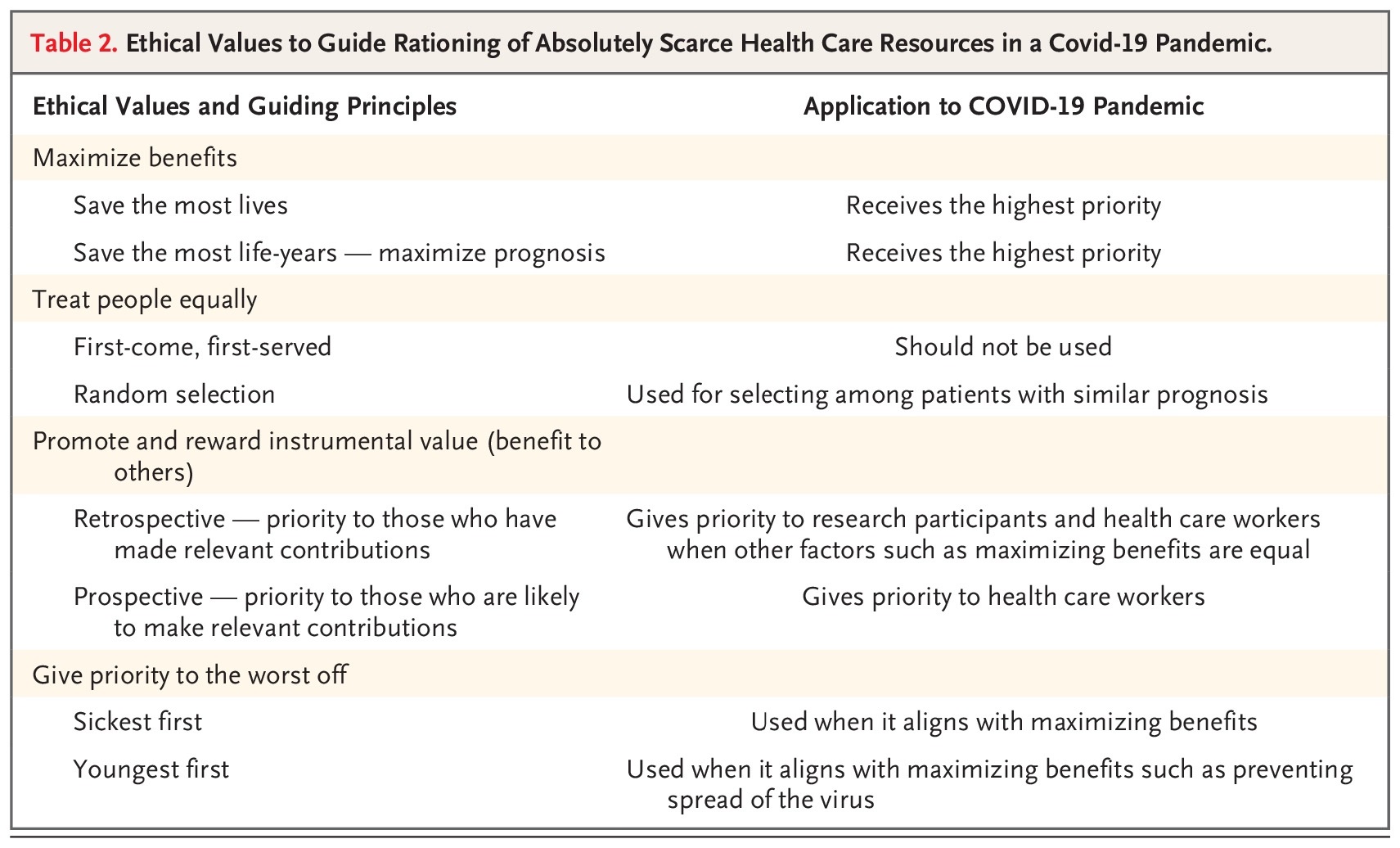
A summary table has been created by Emanuel et. al. of their view of the ethical issues:
Guidance:
Guidance from Royal College of Physicians (UK)
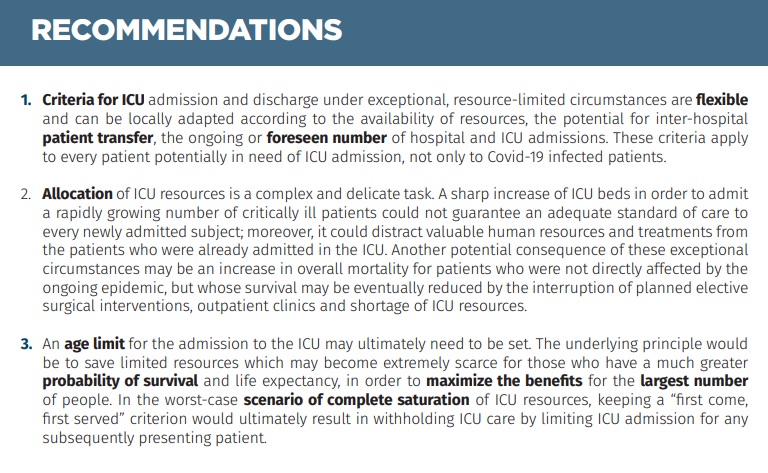
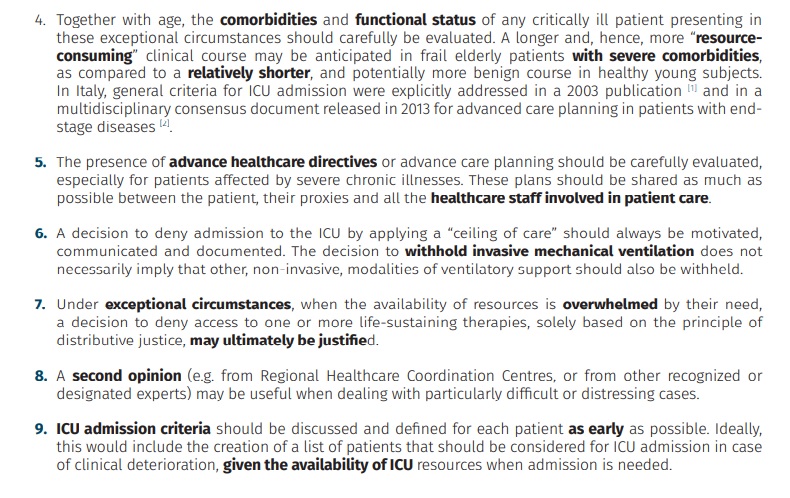
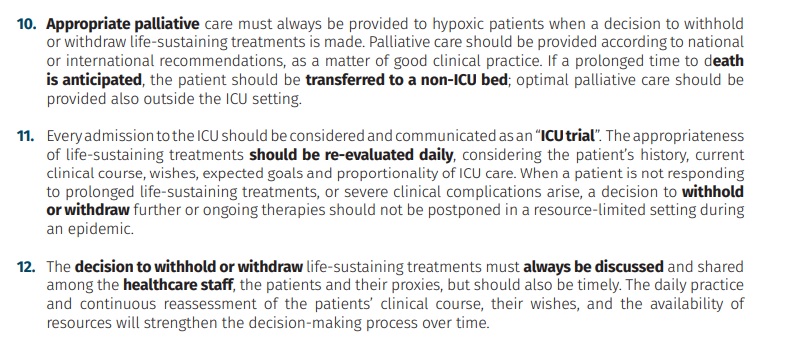
Italian Society of Anaesthesia, Analgesia, Resuscitation and Intensive Care released guidance on "Clinical Ethics Recommendations for the Allocation of Intensive Care Treatments in exceptional, resource-limited circumstances" (5) - which is shown below.
References
1. Rosenbaum L. Facing Covid-19 in Italy - Ethics, Logistics, and Therapeutics on the Epidemic's Front Line. N Engl J Med. 2020 Mar 18. doi: 10.1056/NEJMp2005492. [Epub ahead of print]
2. Emanuel E et. al. Fair Allocation of Scarce Medical Resources in the Time of Covid-19.N Engl J Med. 2020 Mar 23. doi: 10.1056/NEJMsb2005114. [Epub ahead of print]
3. Gostin LO, Friedman EA, Wetter SA. Responding to COVID-19: How to Navigate a Public Health Emergency Legally and Ethically. Hastings Cent Rep. 2020 Mar 26. doi: 10.1002/hast.1090. [Epub ahead of print]
4. Truog RD, Mitchell C, Daley GQ. The Toughest Triage - Allocating Ventilators in a Pandemic. N Engl J Med. 2020 Mar 23. doi: 10.1056/NEJMp2005689. [Epub ahead of print]
5. SIAARTI. Clinical Ethics Recommendations for the Allocation of Intensive Care Treatments in exceptional, resource-limited circumstances. Available from: http://www.siaarti.it/SiteAssets/News/COVID19%20-%20documenti%20SIAARTI/SIAARTI%20-%20Covid-19%20-%20Clinical%20Ethics%20Reccomendations.pdf [Accessed 2.4.20]
This article was written by Dr Rachel Coles and editted by Dr Asif Qasim, 2nd March 2020.
Loading Author...
It's tragedy, terrible things to see that happens !!!
Unlike in VN, until now, no one die from covid-19.