COVID-19 Prevention - Personal Protective Equipment (PPE) Advice and Adjuncts

What are the key steps to prevent and minimise your risk of COVID-19 infection? The pandemic has put significant pressure on the international supply chains for protective gowns, masks, and sanitisers. All countries have had to take steps to manage their own resources and supply chains to protect healthcare and front-line workers, as well as the public.
A further challenge in the resource poor setting is the limited access to medical grade protective equipment, disinfectants and a constant water supply. Therefore advice and use of protective equipment in low-income countries may have to adapt to local availability of resources.
What practical steps could help healthcare workers minimise exposure during this ?
“We would continue to recommend the use of a barrier in addition to PPE. It is critically important to use every possible measure to ensure patient safety while protecting health care personnel from exposure to this highly contagious infection.”
From Rafael Ortega, M.D., Ala Nozari, M.D., Ph.D. and Robert Canelli, M.D., Boston Medical Center, Boston, MA, in response to comment on safety of use of the “Aerosol Box” [1,2]
“Aerosol box”: Innovative enclosure for intubation to reduce risk of COVID-19?
A box to protect staff during intubation, was developed to minimise exposure in settings where levels of PPE are inadequate, in response to the COVID-19 pandemic.
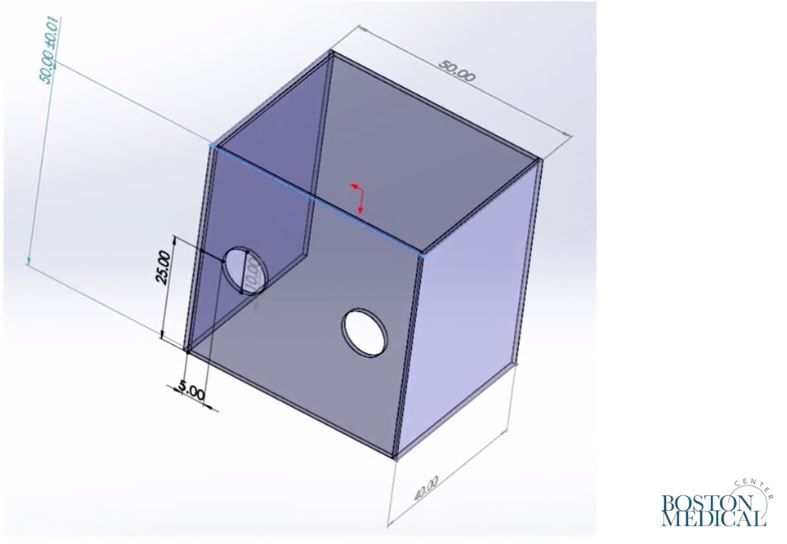
Design first introduced by an Anaesthetist in Taiwan in response to COVID-19

Source: Ortega et. al. (2020)
This “aerosol box” was tested in a simulated environment, and was not validated for the projectile direction, speed, or turbulence of a true cough and may produce more droplets rather than aerosols. Therefore the particle-distribution may not be representative of a true cough.
Nevertheless, the authors suggest this could be an ad hoc barrier enclosure or adjunct to standard PPE. However, the authors found that the box restricted hand movement and would require training before use in the treatment of patients. Operators should be ready to abandon use of the box should airway management prove difficult.
This adjunct has faced criticism that it poses an additional surface of contamination and decreases safety[2]. See the discussion here.
Clear plastic drapes to create a physical barrier
It is clear that one way to reduce transmission is to recognise the potential scenarios and procedures where health care workers will encounter droplets and aerosols from a potential COVID-19 patient and take measures to reduce risk.
Clear plastic drapes have been used in airway procedures before the pandemic, such as tracheostomy formation, to allow visualisation of the operative field by the anaesthetist standing at the head-end of the patient.
Sterile drapes have been used for surgery and procedures, and is well established to minimise contamination via surface contact, with healthcare settings using a range of products which may be single-use or disposable, or adhesive or non-adhesive [4]. While not all materials eliminate aerosols and droplets, they provide a physical barrier which prevents surface contamination.
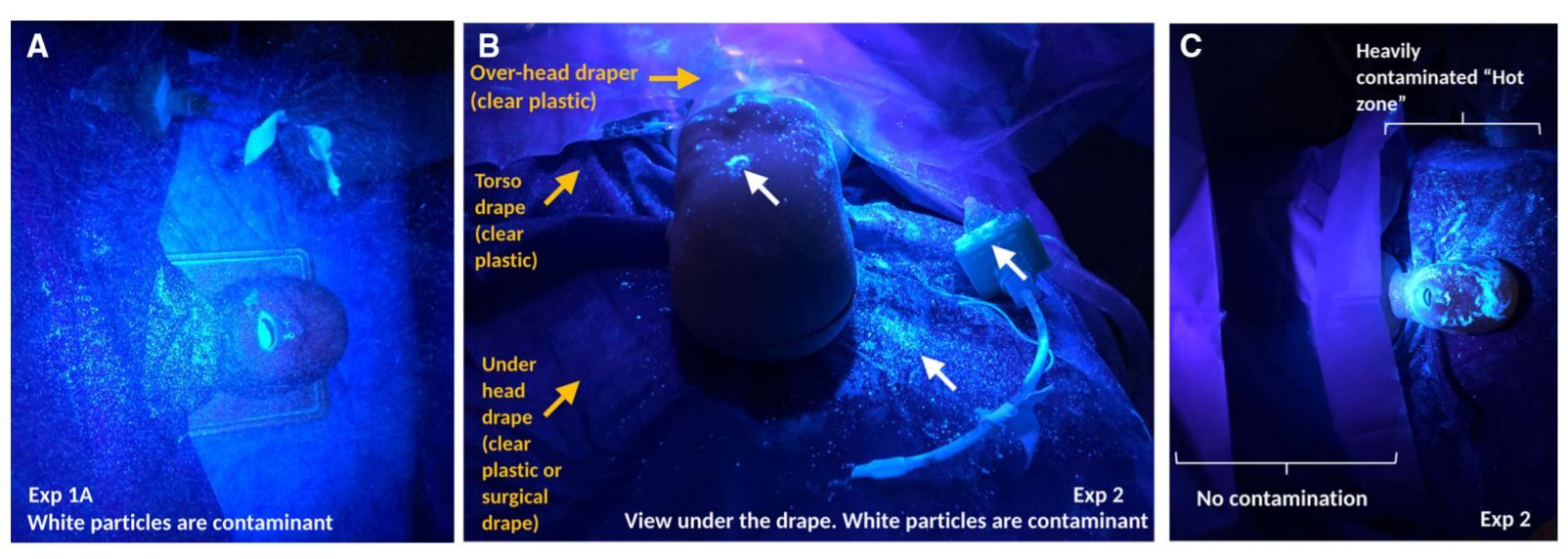
Source: Matava et.al. (2020)
Here is a 3-layer technique using plastic drapes for intubation described by Matava et.al. (2020)[3]:
1) First layer was placed under the head to protect the operating table and linen
2) Second layer torso-drape layer was applied from the neck down and over the chest, preventing contamination of the upper torso
3) Third over-head top drape was a clear plastic drape with a sticky edge that was secured at the mid-sternum level. It was draped over the patient’s head to prevent contamination of the surrounding surfaces, including the HCPs
4) After the cough generating procedure was complete, the top two drapes were rolled away together toward the patient’s legs to contain and remove the contaminant, and the third drape was removed afterwards
A mismatch of supply and demand of adequate protective equipment is a challenge faced by many countries, and is not limited to low-income countries. Therefore in the healthcare setting, rationale use of equipment should be taken. View guidance from the WHO here.
What do you think of the existing advice and what measures have you seen in practice that may be helpful, either in the healthcare setting or in the community?
We are interested in hearing your comments and add to the discussion on MedShr.
Useful Resources on Protective Equipment for the Healthcare setting:
Why should Healthcare Professionals wear FFP masks?
How to fit check your FFP mask
UV light shows potential use of protective airway enclosures
FFP3 Mask associated Headaches
Should we re-use N95 FFP masks?
WHO: Coronavirus disease (COVID-19) technical guidance
References:
Ortega R, Nozari A, Canelli R, April 3, 2020, Correspondence: Barrier Enclosure during Endotracheal Intubation DOI: 10.1056/NEJMc2007589
Ortega R, Nozari A, Canelli R, May 5, 2020, Response to Letter to the Editor (Published online) Website:https://www.nejm.org/doi/full/10.1056/NEJMc2012960?query=recirc_curatedRelated_article (accessed 11/5/2020)
Matava CT, Yu J, Denning S. Clear plastic drapes may be effective at limiting aerosolization and droplet spray during extubation: implications for COVID-19 [published online ahead of print, 2020 Apr 3]. Can J Anaesth. 2020;1‐3. doi:10.1007/s12630-020-01649-w
Webster J, Alghamdi A. Use of plastic adhesive drapes during surgery for preventing surgical site infection. Cochrane Database Syst Rev. 2015;2015(4):CD006353. Published 2015 Apr 22. doi:10.1002/14651858.CD006353.pub4
Loading Author...
Sign in or Register to comment