COVID-19 Resource allocation: Who should get masks?

Although health care workers are likely to be one of the highest risk groups in terms of exposure, they are also more likely to be trained in the use of masks and fit tested than the general public. With the supply of PPE unable to meet demands, should countries reserve the use of masks for healthcare workers?
What can we do to manage this resource?
Could home-made or improvised masks help protect and prevent the transmission of COVID-19 in the general population?
‘WHO stresses that it is critical that medical masks and respirators be prioritized for health care workers’
The WHO guidance on masks-wearing (Published 6 April 2020) [1]
Coughing and Aerosols: Sequential Schlieren Images of a Cough (NEJM)
Visualising the aerosol generation of a cough - should we mask up?
For any type of mask, appropriate use and disposal are important to prevent COVID-19 transmission through handling of contaminated materials.
Mask Management Concerns – From WHO interim guidance [1]
· Self-contamination from touching and reusing contaminated mask
· Depending on type of mask used, potential breathing difficulties
· False sense of security – reduced adherence to other preventive measures (e.g. physical distancing, hand hygiene)
· Diversion of mask supplies and consequent shortage of mask for healthcare workers
· Diversion of resources from effective public health measures (e.g. hand hygiene)
What is the evidence of wearing cloth masks?
Evidence on resource management and alternative solutions such as homemade masks can be found in existing literature; research and modelling studies to deal with infection outbreaks. This is particularly relevant for low and middle income countries where expensive single use masks and other forms of PPE are not readily available and allocation of funds are finite.
With the likely protracted course of this pandemic, in addition to the healthcare sector, members of the public worldwide will also feel the financial burden of these resources.
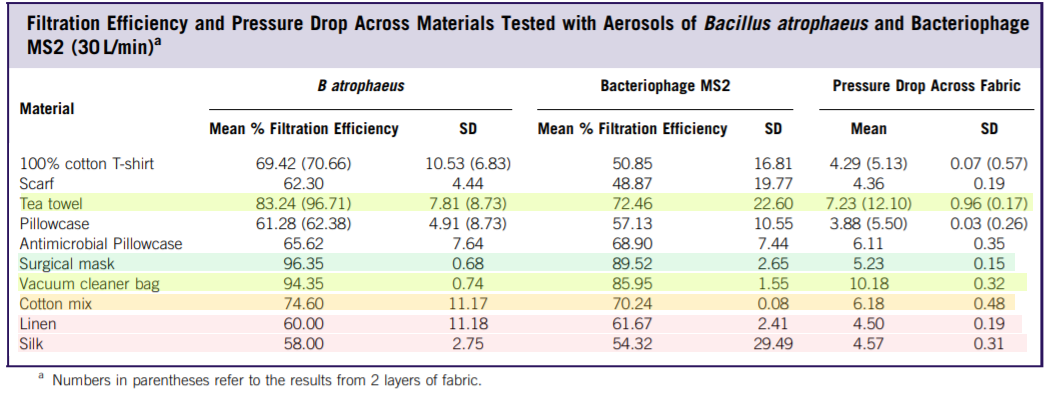
Davies et al. (2013) [2] looked at how well different materials, used for home-made face masks can prevent droplet transmission, for example for use in a pandemic. The how well masks fit and the reduction of bacteria and droplets measured. Their conclusions were that although there was reduction in transmission, this should only be used as a last resort but would be better than no protection at all.
Konda et al. (2020) [3] conducted studies on different fabric materials and combinations to determine the filtering efficacy, which may shed light on which materials would suit a homemade mask for the COVID-19 pandemic. They used an experimental design with an aerosol generator to created particles in the range of a few tens of nanometers to approximately 10 μm.
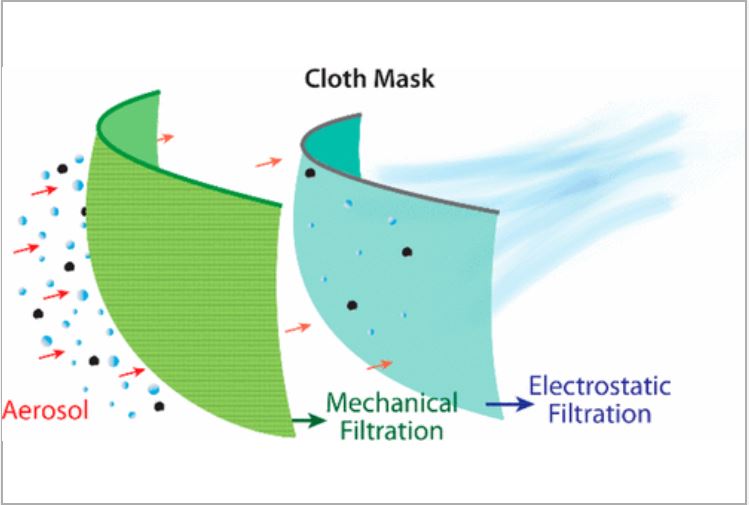
Source: Konda et al. (2020) [3]
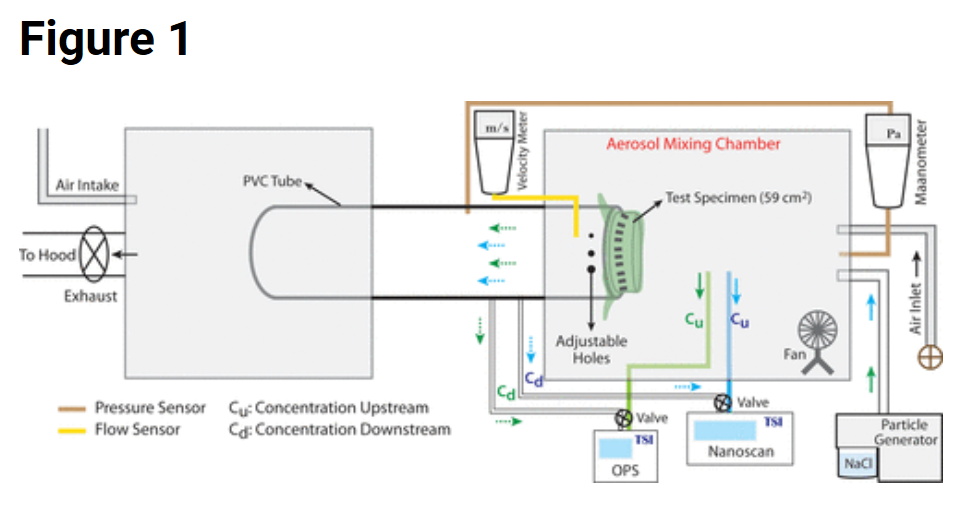
Source: Konda et al. (2020) [3]
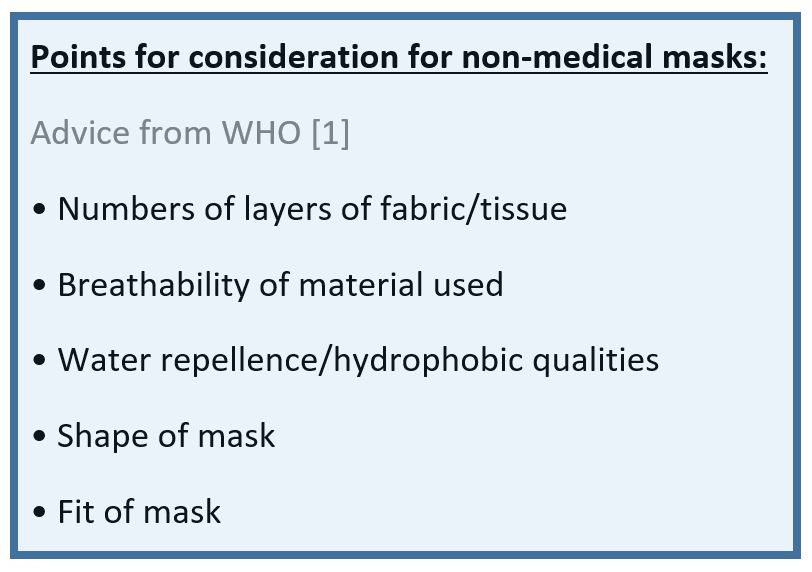
Observations on cloth mask design from Konda et al. (2020):
• Fabric with higher thread count and low porosity (e.g. 600 TPI cotton) filtered better
• Natural silk, chiffon (90% polyester, 10% spandex) and flannel (65%cotton, 35% polyester) could provide good electrostatic filtering
• Multiple layers (e.g. 4 layers of silk) provided good protection in the 10 nm to 6 μm range
• These results do not take into account air leaks from gaps due to lack-of fit (which will reduce the efficacy significantly)

Conclusions:
The use of cloth non-medical masks are likely to become more widespread throughout the world but this should not lull the public into a false sense of protection or immunity. The general public should still observe public health principles of hand hygiene, isolation of unwell or symptomatic individuals and physical distancing until more is known about COVID-19 treatment and prevention.
Useful Resources:
COVID-19 Prevention - Personal Protective Equipment (PPE) Advice and Adjuncts
Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19)
Should we re-use N95 FFP masks?
WHO: Coronavirus disease (COVID-19) technical guidance
Spotlight on Interviews: Practical Aspects of Otolaryngology Services During the COVID-19 Epidemic
References:
1. WHO, 6 April 2020, Advice on the use of masks in the context of COVID-19 - Interim guidance, URL: https://www.who.int/publications-detail/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak (accessed 13 May 2020)
2. Davies, A., Thompson, K., Giri, K., Kafatos, G., Walker, J., & Bennett, A. (2013). Testing the Efficacy of Homemade Masks: Would They Protect in an Influenza Pandemic? Disaster Medicine and Public Health Preparedness, 7(4), 413-418. doi:10.1017/dmp.2013.43
3. A Konda, APrakash, G A Moss, M Schmoldt, G D Grant, S Guha, April 2020, Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks, ACS Nano Article ASAP, DOI: 10.1021/acsnano.0c03252
Loading Author...
Sign in or Register to comment